|
Back to Fall Congress
Natural History of the Multicystic Dysplastic Kidney - a Large Single-Center Experience
Adam B. Eickmeyer, Undergraduate pursuing Bachelor of Science, Jonathan R. Dillman, MD, Chang He, M.A., Ethan Smith, MD, Nina F. Casanova, MD, David A. Bloom, MD.
University of Michigan Health System, Ann Arbor, MI, USA.
BACKGROUND: Imaging of patients with multicystic dysplastic kidney (MCDK) has increased over the past three decades. This increased use of imaging provides additional insights into the natural history of MCDK. Our study looked at this data for predictors of involution and associated anomalies.
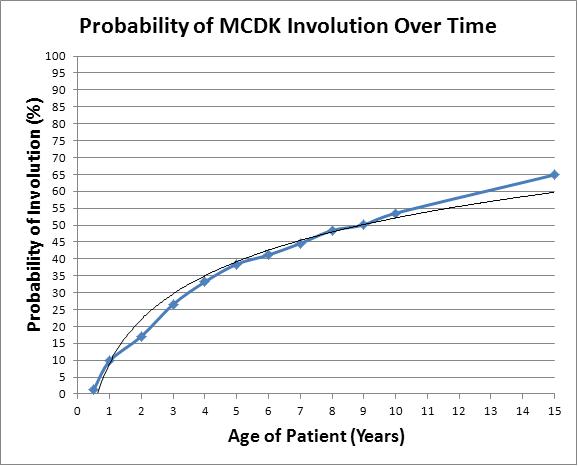
METHODS: University of Michigan Departments of Urology and Radiology records were searched from 1980 to present to identify unilateral MCDK patients. Available radiologic, clinical, and surgical records were reviewed. Demographic information, pertinent radiologic data from ultrasound, CT, MRI, and scintigraphy (laterality, baseline size, size at follow-up imaging, associated anomalies); and antenatal history were documented. Bivariate and multivariate analyses were performed to identify predictors of MCDK involution. Subjects with baseline renal imaging within the first year of life and subsequent follow up imaging at least one year later were included in this analysis. Probability of involution over time was assessed using the Kaplan-Meier method.
RESULTS: 301 unilateral MCDKs were identified. 195 (64.8%) were detected antenatally. 136 (45.2%) MCDKs were in girls. 160 (53.2%) MCDKs were right-sided. Mean size at baseline imaging was 5.0 ± 0.2 cm (Mean ± SE). Associated abnormalities included contralateral ureteropelvic junction obstruction (N=10; 3.3%), contralateral ureterovesical junction obstruction (including primary megaureter) (N=6; 2.0%), ipsilateral vesicoureteral reflux (VUR) (N=21; 7.0%), contralateral VUR (N=63; 20.1%), and renal fusion anomaly (N=4; 1.3%). 68 subjects were excluded from our analysis of predictors of involution. Of the 233 remaining subjects, the cumulative probability of involution was 9.8% at 1 year, 38.5% at 5 years, and 53.5% at 10 years of age. Baseline MCDK size was the only significant predictor of involution at bivariate (p<0.0001) and multivariate (p<0.0001; OR 0.58 [95% CI: 0.49, 0.69]) analyses. Patients that experienced involution had a mean initial MCDK size of 3.8 ± 0.3 cm (mean ±SE) while patients that did not experience involution had a mean initial size of 5.8 ± 0.2 cm. Laterality, gender, associated renal/genitourinary tract abnormalities, and antenatal vs. prenatal diagnosis were not found to be significant predictors of involution. No MCDK developed malignancy during the study period. 9, 24, and 15 MCDKs were surgically resected between 1980-1989, 1990-1999, and 2000-present, respectively.
CONCLUSIONS: MCDK is a condition with no validated algorithm for treatment. Our study found that children with initially smaller MCDKs are more likely to experience involution. We found that approximately 53.5% of children with MCDK experience involution by age 10. If one were to extrapolate our data out into the future, it might appear that most would regress by age 30 years. For the few that do not totally involute, malignancy in MCDK is rare and hypertension is uncommon. Calcification of the cysts and traumatic injury are of course possibilities, but we see no absolute indication for nephrectomy in infants or older children with MCDKs.
Back to Fall Congress
|

