|
Back to Fall Congress
Clinically Relevant Diagnostic Pitfalls Associated With Reliance on Ultrasound Evaluation to Guide Management of Suspected Cryptorchidism
Niki Kanaroglou, MD, FRCSC, Elias Wehbi, MD, FRCSC, Joseph Gleason, MD, Darius Bagli, MD, Joao Pippi Salle, MD, Martin Koyle, MD, Armando J Lorenzo, MD.
The Hospital for Sick Children, Toronto, ON, Canada.
BACKGROUND:
The diagnostic inaccuracy of ultrasound (US) evaluation for undescended testes (UDT) is becoming increasingly clear in the literature. When US is used to guide surgical management decisions, false positive and negative results can confuse parents and misinform surgeons. Herein we characterize common diagnostic pitfalls associated with this practice.
METHODS:
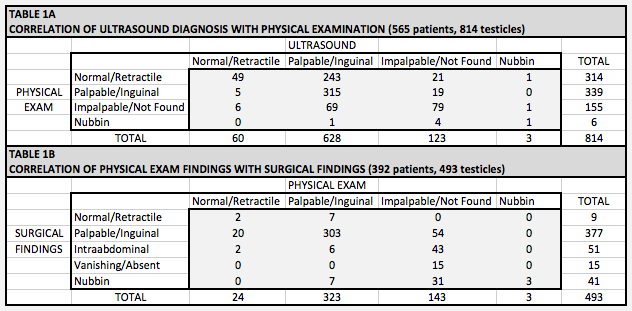
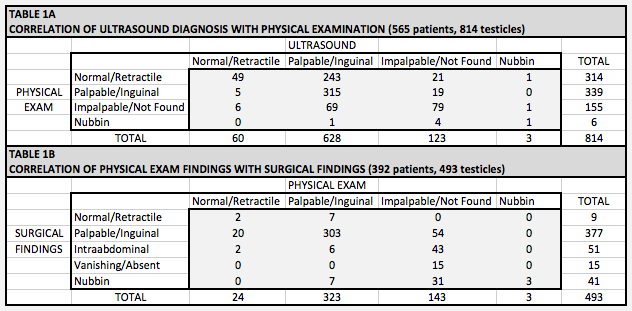
Consecutive referrals for UDT to a major tertiary care institution between 2007-2011 were evaluated, focusing on children assessed after diagnostic US. The results of US evaluation were correlated with findings on physical examination (PE) by a specialist in clinic and during surgery for those who underwent exploration. PE and surgical findings were also correlated. Frequency and patterns of diagnostic errors on US and PE were identified, employing surgical exploration as the ultimate gold standard.
RESULTS:
During the study period 565 patients (814 suspected UDT) were seen in clinic, 44% (249/565) with reported bilateral pathology. All patients had at least one US ordered by the referring practitioner prior to assessment. Of these, 69% (392/565) underwent surgical exploration. Pertinent data is shown in Table 1. Importantly, US correctly predicted PE findings in only 54% (439/814) of cases, while PE correctly determined testicular location in 81% (397/493). In 84% (265/314) of testicles with a normal exam, US incorrectly diagnosed an UDT. In addition, 20/56 (36%) explorations demonstrating an absent or atrophic testicle, US incorrectly diagnosed the presence of a gonad.
CONCLUSIONS:
This large review confirms the diagnostic inaccuracy of US for UDT and highlights potentially troublesome errors that may mislead parents and physicians, with important medico-legal implications. Physical examination by an experienced practitioner shows a stronger correlation with definitive surgical findings than US, making it the most accurate and effective way of evaluating children with cryptorchidism.
Back to Fall Congress
|