|
Back to Fall Congress
Cost Analysis Of Prophylactic Antibiotics Vs. Placebo To Prevent Urinary Tract Infections In Infants With High Grade Hydronephrosis
Julia Pemberton, MSc, PhD(c)1, Armando J. Lorenzo, MD2, Luis H. Braga, MD, MSc, PhD1.
1McMaster University, Hamilton, ON, Canada, 2The Hospital for Sick Children, Toronto, ON, Canada.
BACKGROUND:
Hydronephrosis (HN) is one of the most common congenital anomalies. Urinary stasis and associated impaired drainage in hydronephrotic kidneys may predispose patients to febrile urinary tract infections (UTI). Antibiotic prophylaxis (ABP) has been recommended for newborns with HN to reduce the rate of UTI, nevertheless its use remains controversial. To date an economic evaluation of ABP has not been conducted in this population. Herein we evaluated if ABP (versus No ABP) is an efficient use of limited healthcare resources, given costs and consequences, to treat children with high grade HN within the first two years of life.
METHODS:
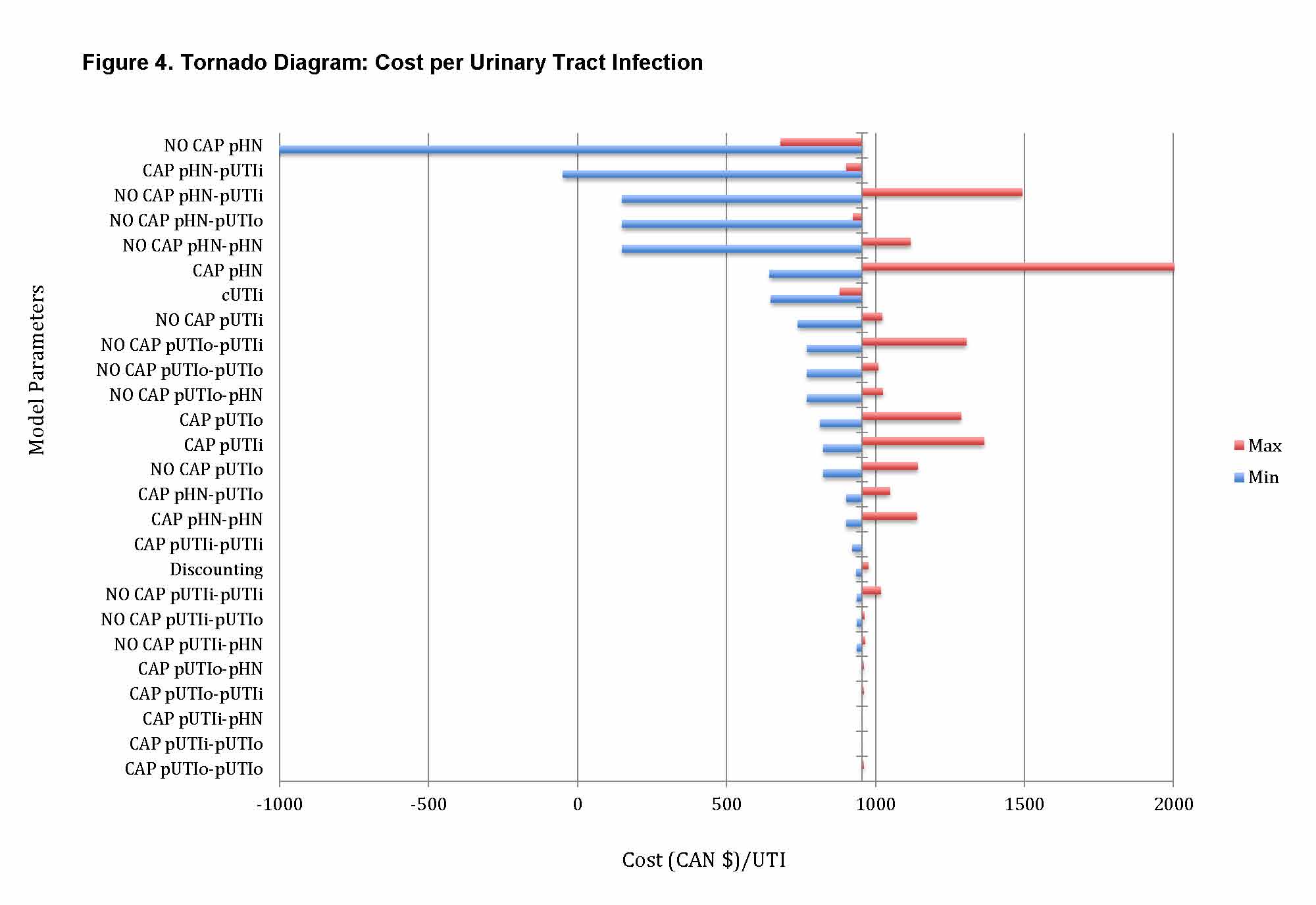
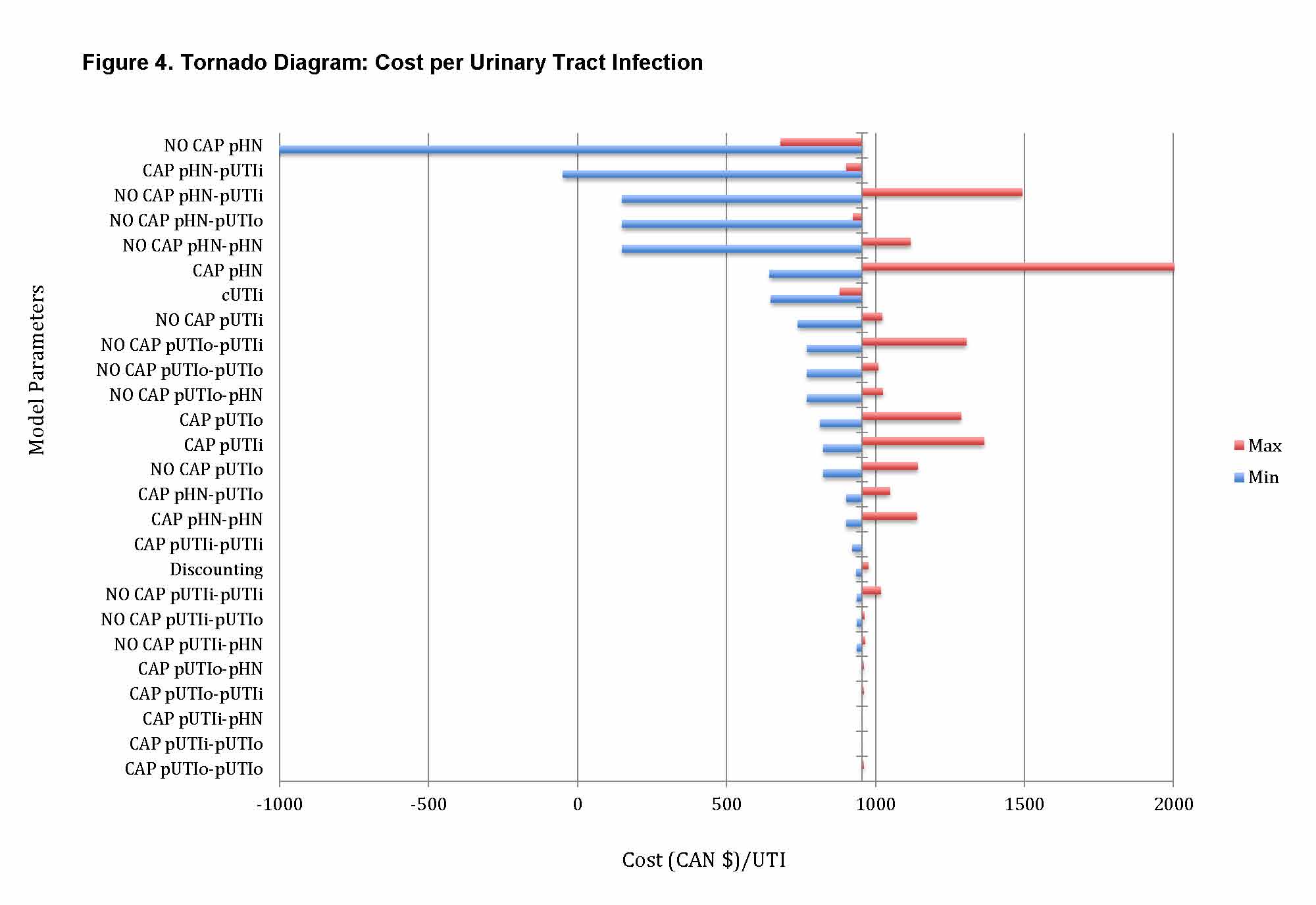
A probabilistic decision model was used to estimate expected costs, outcomes and Quality-Adjusted Life Years (QALYs) of the two treatment options (ABP versus No ABP). Cost data were collected from provincial databases and corrected to 2013 Canadian dollars. Estimates of risks and health utility values were extracted from the literature. Assumptions on ABP benefit were obtained from a contemporary systematic review on the topic. Cost-effectiveness was expressed as dollars per UTI and dollars per UTI requiring hospitalization. Cost-utility was expressed as dollars per QALY. The analysis was performed from a third party payer perspective with a time horizon of two years. One-way sensitivity analysis was performed to assess uncertainty and robustness of our model. RESULTS:
Overall ABP is less costly and provides an increase in health utility when compared to no ABP in this population. Given this dominance of ABP over no ABP, calculation of incremental cost effectiveness was not warranted. The mean annual costs for ABP was $1,414.06 (versus $1,685.56 for no ABP), with a reduction of 0.28 UTIs per year, and 0.04 UTIs requiring hospitalization per year. Cost-utility analysis revealed an increase of 0.62 QALYs/year when using ABP versus not. ABP continued to be more cost-effective over the no ABP in all one-way sensitivity analyses.
CONCLUSIONS:
This probabilistic model provides a robust Canadian-specific assessment of two cost effectiveness and one cost utility measure. Based on our data, across all three outcomes ABP is a better use of healthcare resources when compared to no ABP in infants with high-grade hydronephrosis to prevent UTIs within the first two years of life.
Back to Fall Congress
|