|
Back to Fall Congress
Prospective Single Center Analysis on the Diagnostic Performance of Measurements of the Normally Descended Gonad in Predicting Monorchidism in Boys with Unilateral Non-palpable Testis
Luis H. Braga, MD, MSc, PhD1, Forough Farrokhyar, PhD1, Armando J. Lorenzo, MD2.
1McMaster University, Hamilton, ON, Canada, 2The Hospital for Sick Children, Toronto, ON, Canada.
BACKGROUND:
There are limited data on the relationship between contralateral compensatory testicular hypertrophy and monorchidism, with only a handful of relatively small case series published on the topic. To provide further information on the prognostic value of testicular measurement we designed a prospective study with the specific aim to identify a cut-off size for the compensatory hypertrophic testis that would assist in predicting monorchism (intra-abdominal vanishing testis or inguinal/scrotal nubbin) in patients with unilateral nonpalpable testis (NPT).
METHODS:
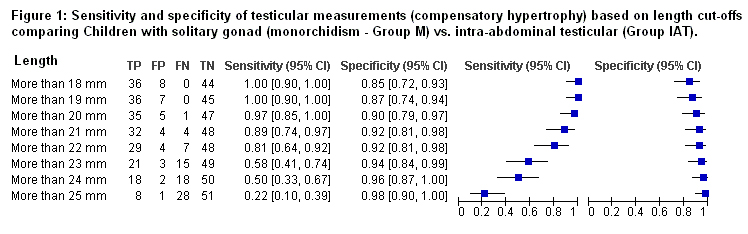
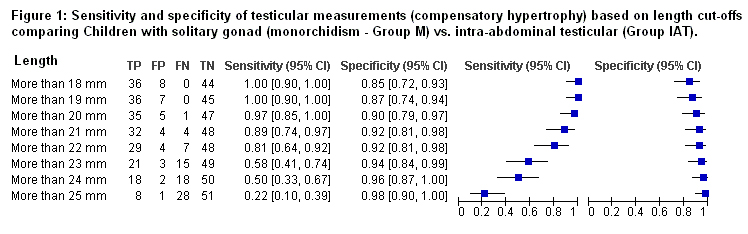
Between 2009 and 2013, all patients with cryptorchidism treated by a single surgeon at a tertiary care center were assessed. Patients were segregated into groups based on intra-operative findings: children with a solitary gonad (monorchism group, M) and two control groups (boys with intra-abdominal testis [IAT] and those with palpable undescended testis [pUDT]). Children with retractile, bilateral undescended, ascending testes and those >5 years of age were excluded. The same individual prospectively collected standardized measurements of contralateral descended testes (length and width) using a caliper, with the child under anesthesia, immediately before the start of the procedure. By protocol, all NPT patients underwent diagnostic laparoscopy. In cases with the vas and vessels seen entering the internal inguinal ring an inguinal incision was carried out to confirm the diagnosis and remove any inguinal or scrotal nubbin. Alternatively, laparoscopic or open orchidopexies were performed depending on testicular location. Sensitivity, specificity, positive and negative predictive values, likelihood ratios and receiver operating characteristic (ROC) curves were calculated.
RESULTS:
Out of 254 boys with cryptorchidism 166 were found to have a pUDT and 88 a NPT. Of these 88 NPT patients, 52 had an IAT and 36 monorchism. Mean ages at surgery for groups M, IAT and pUDT were similar (31.2, 31.2 and 34.4 months, respectively; p=0.2). Mean length of the contralateral descended testes in groups M, IAT and pUDT was 24.9, 16.5 and 18.0mm, respectively (p18, >19 and >20mm (6.25, 7.4 and 12.6 respectively). Finally, the area under the ROC curve was 95.3% (95%CI: 91-100%), confirming the accuracy of the 20mm cut-off point in predicting monorchism.
CONCLUSIONS:
Based on this prospectively collected data on consecutive boys with cryptorchidism we corroborate the predictive value of testicular hypertrophy in determining the likelihood of having a vanishing or atrophic testicle.
A cut-off length of 20mm for the descended gonad serves as an important threshold, as it carries a high sensitivity, specificity and likelihood ration in suspecting monorchism. If validated, this information will serve as an important clinical parameter to provide preoperative counselling and plan surgical approach in this patient population.
Back to Fall Congress
|