|
Back to Fall Congress
Tower Uroflow Pattern: How often is it seen in Children with Detrusor Overactivity (DO)?
Jason P. Van Batavia, MD, Andrew J. Combs, RPA-C, Kenneth I. Glassberg, MD.
Division of Pediatric Urology, Morgan Stanley Children's Hospital of New York-Presbyterian Hospital, Columbia University, New York, NY, USA.
BACKGROUND: Uroflow patterns are often used to support presumptive diagnoses and initiate therapy. For instance, a tower flow pattern (left shifted explosive curve with peak flow almost immediately after start of flow) is thought to be indicative of detrusor overactivity (DO). Despite this presumed association, it is unknown how many children with DO will actually have a tower pattern. We previously reported that children with idiopathic detrusor overactivity (IDO) when voiding with urgency have an EMG lag time of ≤0 seconds on uroflow/EMG. This EMG lag time cut-off has a high specificity for documented DO making it a reasonable surrogate for urodynamics in detecting its presence. (J Urol June, 2013) In this study, we sought to determine the spectrum of uroflow patterns at presentation for these children diagnosed with IDO and a quiet pelvic floor EMG when voiding.
METHODS: We reviewed our pediatric lower urinary tract dysfunction database for patients diagnosed with IDO and limited inclusion to only those with an EMG lag time ≤0 seconds and a quiet EMG during voiding. Presenting LUTS and uroflow patterns, as per ICCS guidelines, both at diagnosis and on-treatment were reviewed.
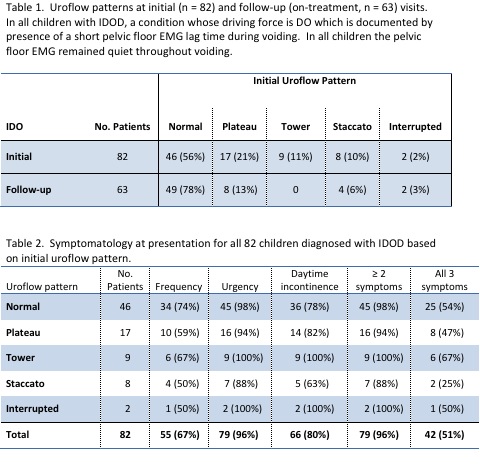
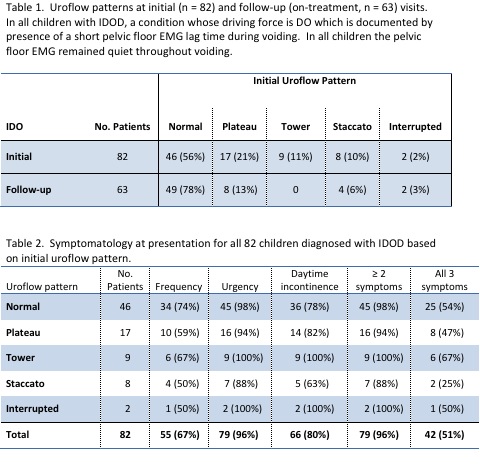
RESULTS: 82 children (46M, 36F; mean age 7.4 years, range 4-16) diagnosed with IDO were identified. Initial uroflow patterns in all children and on-treatment uroflow patterns in 63 children with follow-up are shown in table 1. No patient with plateau pattern was found to have urethral obstruction. Presenting symptomatology for all children and for each uroflow pattern are shown in table 2. Only 9 patients (11%) had an initial tower flow pattern and all reverted to normal flow curves on follow up uroflow/EMG studies after their IDO had been effectively treated.
CONCLUSIONS: Most children with IDO at the time uroflow/EMG is performed as evidenced by a very short EMG lag time and a quiet EMG during voiding do not exhibit a tower uroflow pattern, the specific pattern thought to be indicative of IDO and the symptom syndrome called OAB. Although not statistically significant, those with a tower pattern appeared to be the most symptomatic. While a normal uroflow pattern was most common in IDO, 33% had flow curves often thought reflective of other LUT conditions and should serve as a cautionary note against relying on specific flow patterns alone to diagnose their underlying condition.
Back to Fall Congress
|