|
Back to Fall Congress
Uroflow Patterns in Patients with Dysfunctional Voiding
Kenneth I. Glassberg, MD, Sven Wenske, MD, Jason P. Van Batavia, MD, Andrew J. Combs, RPA-C.
Division of Pediatric Urology, Morgan Stanley Children's Hospital of New York-Presbyterian Hospital,, New York, NY, USA.
BACKGROUND: Although a staccato uroflow pattern is generally presumed to be indicative of dysfunctional voiding (DV), we recently reported that when uroflow is performed with simultaneous pelvic floor electromyography (uroflow/EMG), only 1/3 of children with staccato pattern had documented DV with an active pelvic floor EMG during voiding. In this study we aimed to determine the reverse, ie how often does a staccato uroflow pattern occur in children diagnosed with DV. In addition, we sought to determine what other uroflow patterns are prevalent during voiding in children with DV and what if anything happens to the uroflow pattern after DV has been corrected.
METHODS: We reviewed our pediatric lower urinary tract (LUT) dysfunction registry for patients with EMG documented DV. Uroflow patterns at initial presentation were recorded and categorized as either staccato, interrupted/fractionated, mixed staccato/interrupted or bell shaped as defined by the ICCS. All patients received biofeedback and standard urotherapy. Patients with significant associated overactivity also received anticholinergics. Flow patterns following successful correction of DV as measured on follow-up uroflow/EMG were assessed.
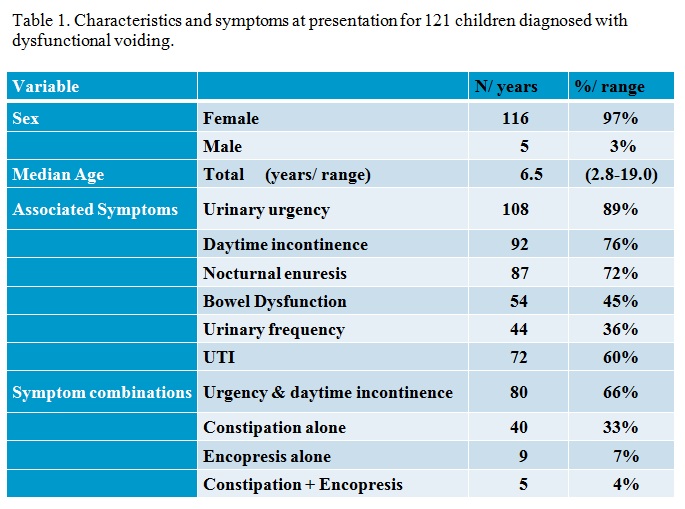
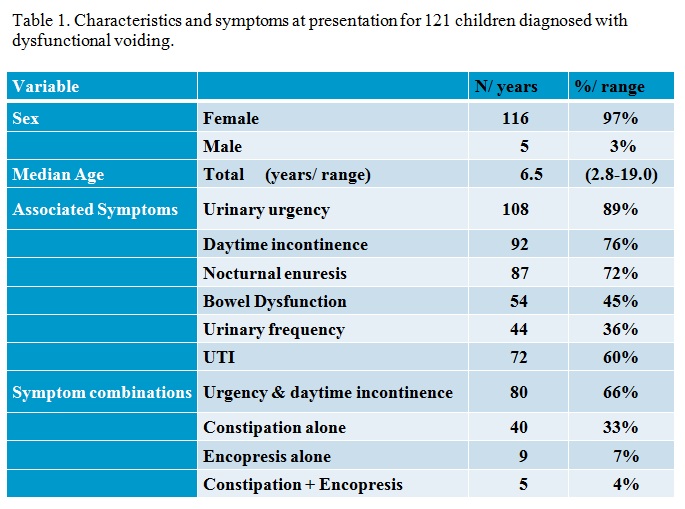
RESULTS: Of 596 children entered into the LUTD database,121 had an active pelvic floor EMG during voiding, consistent with a diagnosis of DV. A staccato uroflow pattern was present in 70 (58%); 22 (19%) had interrupted/fractionated pattern, 12 (10%) had a mixed pattern and 17 (14%) had a bell shaped though typically depressed pattern. Most prevalent associated symptoms are shown in table 1. Following successful treatment of DV with documented quiet EMG during voiding on follow up uroflow/EMG, 96.3% of all those with any form of staccato pattern and 80% of those with initial interrupted pattern converted to a normal bell shape curve. Despite correction of DV, 45% had a short EMG lag time (<2 seconds) suggesting residual detrusor overactivity on follow up.
CONCLUSIONS: In patients with EMG documented DV, staccato flow was indeed the most common flow pattern but present in less than two-thirds, while nearly a third had some variant of interrupted flow, a pattern thought by some not to reflect DV at all. Most importantly, successful, documented correction of DV results in the conversion of grossly abnormal flow patterns into normal bell shaped curves in the vast majority of cases and underscores the importance of assessing flow with simultaneous pelvic floor EMG.
Back to Fall Congress
|