|
Back to Fall Congress
Is microscope repair of distal hypospadias superior to loupe magnification?
Mark R. Zaontz, MD, Bic N. Cung, MD, Gregory E. Dean, MD, Michael G. Packer, MD, Jonathan A. Roth, MD.
Temple, Philadelphia, PA, USA.
Background:
Hypospadias surgery lacks standardization of reporting and long term follow-up data. We report outcomes for distal Thiersch Duplay hypospadias repair utilizing a single institution database. We hypothesize that the use of the operating microscope will reduce complications compared to loupe magnification.
Methods:
We retrospectively reviewed our single institutional database for all distal Thiersh-Duplay (TD) hypospadias repairs in prepubertal boys between 2002 and 2011. All surgeries were performed by four senior pediatric urologists, one of whom exclusively utilized microscope magnification (6-10x) while the other three incorporated loupes-assisted magnification (3.5x). Depo-testosterone was given preoperatively to all patients except in those with megameatus intact prepuce (MIP). We analyzed outcomes with respect to magnification techniques. Fisher’s Exact Test was used for statistical analysis.
Results:
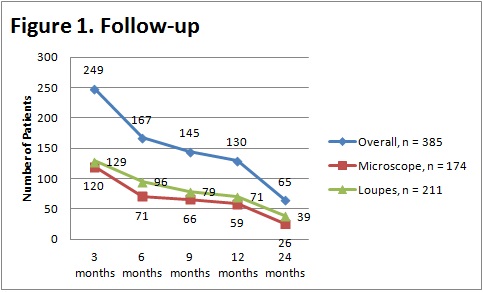
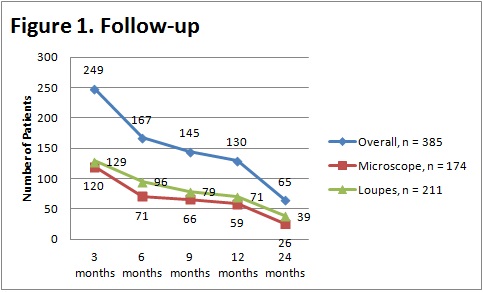
A total of 385 primary TD hypospadias repairs were performed during the inclusion period. Median age at surgery was 8 months (range 4 months - 12 years). The types of hypospadias included subcoronal (45%), distal shaft (18%), coronal (16%), glandular (8%), midshaft (7%), and MIP (6%). There were 32 complications reported (8%): 17 (4%) urethrocutaneous fistulas, 6 (1.5%) meatal recession, 5 (1%) meatal stenosis, and 3 (1%) dehiscence (Table 1). 174 patients had repair utilizing the microscope and 211 had loupes-guided repair. The latter group had more complications, 29 vs. 3 (p<0.0001). The complications after microscope repair included 1 dehiscence (<1%), 1 meatal stenosis (<1%), and 1 (<1%) suture track inclusion. The complications following loupes-guided repair included 17 (8%) fistula, 6 (3%) meatal recession, 4 (2%) meatal stenosis, and 2 (1%) dehiscence (Table 2). Median follow up was 4 months (range 0.1 - 7.6 years).
Conclusions:
Our complication rate was significantly lower when microscope amplification was used, specifically with respect to fistula formation (p<0.0001) and meatal recession (p=0.034). Our preliminary data suggest that distal TD repair with microscope achieves superior outcome compared to loupes magnification - recognizing that length of follow-up as well as surgeon technical nuances are limiting factors of the study (figure 1).
Table 1. Overall Complications | | | Type | Number (%) | | Dehiscence | 3 (1) | | Fistula | 17 (4) | | Meatal stenosis | 5 (1) | | Meatal recession | 6 (1.5) | | Misc. | 2 (<1) |
Table 2. Complication of Microscope vs Loupes
| | | | | Type | Microscope, n=174 (%) | Loupes, n=211 (%) | P | | Overall | 3 | 29 | <0.0001 | | Dehiscence | 1 (1) | 2 (1) | 1.0 | | Fistula | 0 | 17 (8) | <0.0001 | | Meatal stenosis | 1 (1) | 4 (2) | 0.383 | | Meatal recession | 0 | 6 (3) | 0.034 | | Other | 1 (1) | 1 (<1) | |
Back to Fall Congress
|