|
Back to Fall Congress
Clinical and Radiographic Success after Dextranomer/Hyaluronic Acid Copolymer Injection for the Treatment of Vesicoureteral Reflux
Elizabeth Malm-Buatsi, MD, Blake Palmer, MD, Faridali Ramji, MD, Kirk Wettengel, Research Coordinator, Bradley Kropp, MD, Dominic Frimberger, MD.
University of Oklahoma, Oklahoma City, OK, USA.
Introduction/Objectives: The endoscopic injection of dextranomer/hyaluronic acid (Dx/HA) for vesicoureteral reflux (VUR) is thought to be a simple procedure with a short learning curve. Standardized injection techniques have been introduced to achieve consistent results. However, outcomes still vary between 48-92% and there is no real correlation between the clinical and radiological success. We report our radiographic success rate, defined as the absence of VUR on post-operative voiding cystogram (VCUG) and the clinical success rate, defined as the absence of infections off prophylactic antibiotics (PA).
Material and Methods: A retrospective review was performed to evaluate the radiographic and clinical success of Dx/HA injections. From 2005-2010, injections were carried out using the double hydrodistension implantation technique (HIT). Factors evaluated included gender, age, grade of VUR, pre- and post-operative voiding studies, radiologic findings, repeat surgery and co-morbidities, and post-operative urinary tract infections (UTI). Patients with post-operative VUR that occurred only at supraphysiologic high bladder filling were taken off their antibiotics and followed clinically. Both radiographic successes and failures were followed for UTIs. Patients who did not undergo a post-operative VCUG were followed clinically off PA.
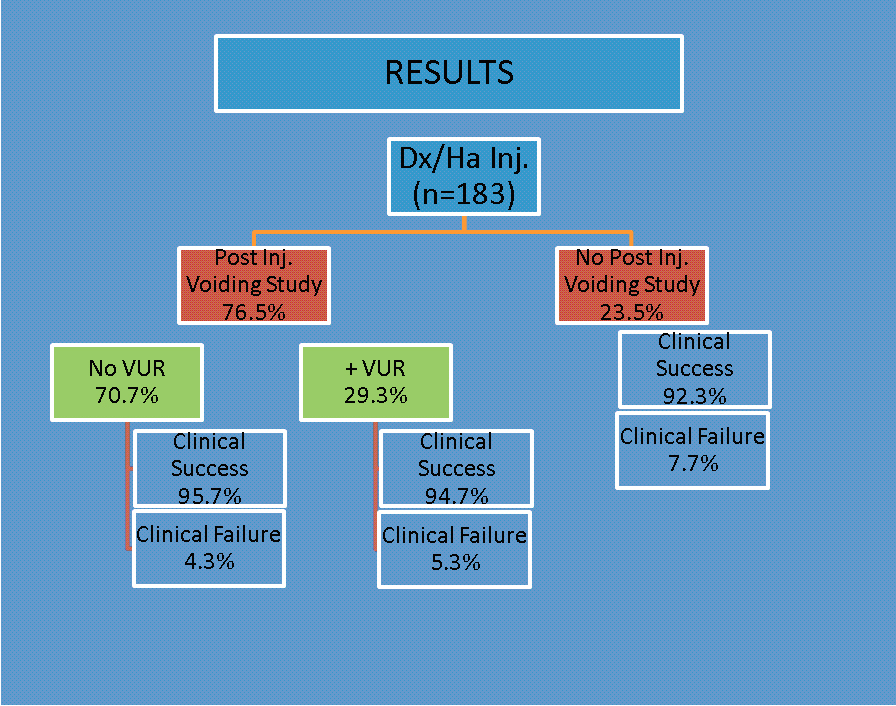
Results: 183 patients were injected, 81.4% females and 18.6% males. Ages ranged from 6 months to 16.5 years and follow- up from 1 to 5 years. Grade distribution was 9.5% grade 1, 31.8% grade 2, 43.8% grade 3, 11.3% grade 4 and 3.6% grade 5. Post-operative VCUG was done in 140 patients (76.5%) and no reflux was seen in 99, for an overall radiographic success rate of 70.7%. Of the radiographic failures, 68.3% had repeat Dx/HA injection, 4.9% underwent open reimplantation and 29.3% were observed off of PA. Of the radiographic successes that were followed for at least 12 months off of PA, 95.7% were clinical success and 4.3% were clinical failures. Of the radiographic failures that were taken off the PA without secondary surgery, 94.7% were a clinical success and 5.3%
were clinical failures. Of the 43 patients who did not undergo a post-operative VCUG, 92.3% were a clinical success.
Figure: Cortisol concentrations. (A) Mean cortisol concentrations (æg/dl) with standard deviations for 260 time points 1-5. (B) Cortisol concentrations (æg/dl) over time for all subjects. Three subjects had outlying 261 values; all underwent minimally invasive procedures. To convert to nmol/L, multiply values by 27.78.
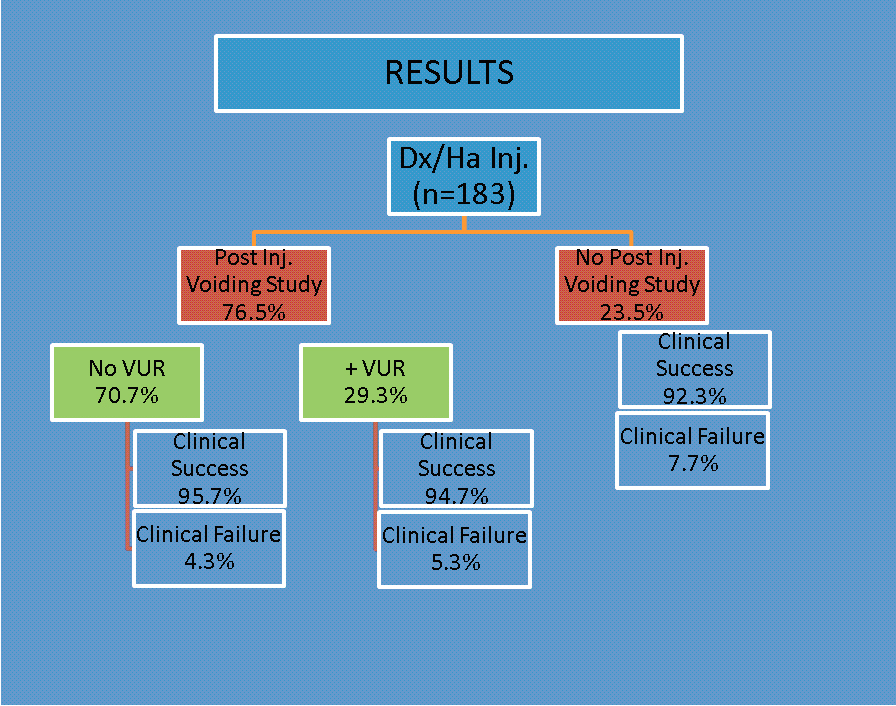
Conclusion: The current group of patients demonstrated a 70.7% radiographic and an overall 94.2% clinical success. Patients that show post-operative VUR only at supraphysiologic bladder fillings in comparison to the preoperative study can be followed clinically off of PA. Secondary surgery should be considered for significant VUR or recurrent infections after surgery. This may factor into the cost consideration in light of increasing healthcare costs.
Back to Fall Congress
|