|
Back to Fall Congress
National Trends and Disparities in the Use of Minimally Invasive Pediatric Nephrectomy
Jack S. Elder, M.D., Jesse Sammon, D.O., Grace Zhu, B.S., Quoc-Dien Trinh, M.D..
Vattikuti Urology Institute, Detroit, MI, USA.
Background: Minimally invasive nephrectomy in the pediatric population may have several advantages over open nephrectomy and the current trends regarding its use have not been studied thus far. The primary objective of this study is to examine the disparities in the usage of minimally invasive nephrectomy and open nephrectomy in the pediatric population by exploring specific patient and hospital characteristics.
Materials and Methods:
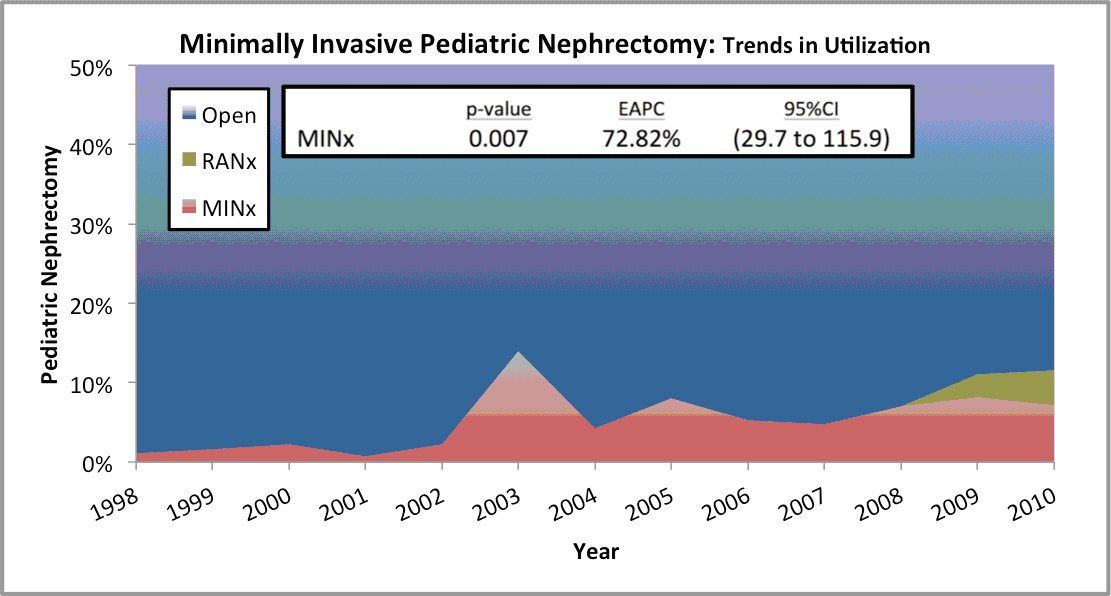
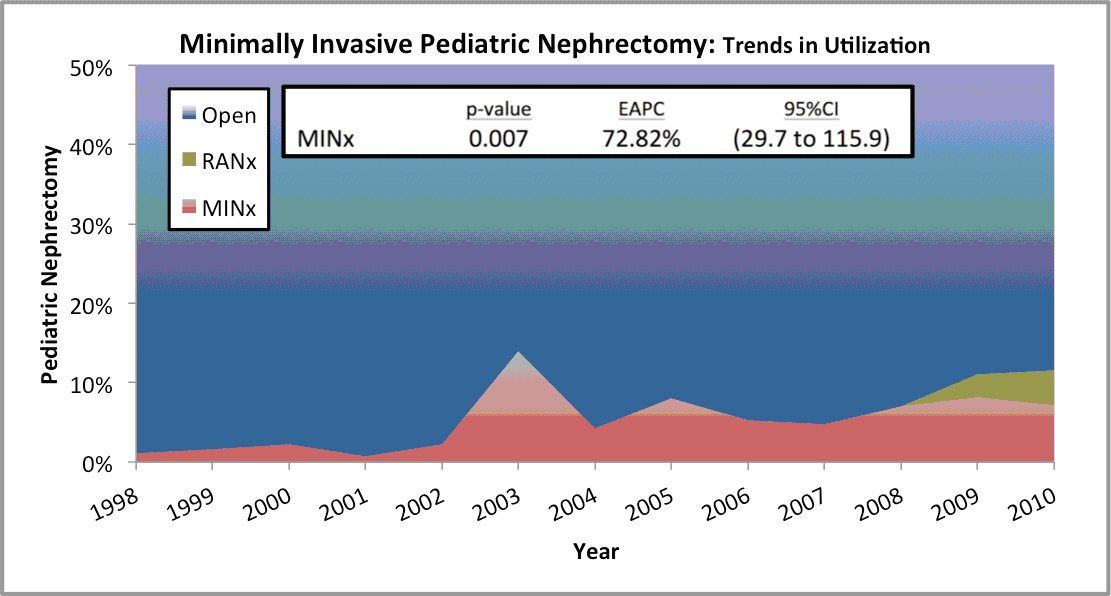
A national estimate of 27,615 pediatric patients treated with nephrectomy by minimally invasive (laparoscopic or robotic) and open approaches between 1998 to 2010 was extracted from the National Inpatient Sample (NIS). The rates of minimally invasive nephrectomy and open nephrectomy were assessed based on year of surgery, patient, and hospital characteristics. The determinants of minimally invasive nephrectomy were evaluated using logistic regression models adjusted for clustering. Trend analysis was performed according to the estimated annual percent change (EAPC) methodology utilizing linear regression.
Results:
Overall, 5.8% of pediatric patients underwent minimally invasive nephrectomy between 1998 and 2010. In United States, the use of minimally invasive nephrectomy increased from 1.1% to 11.6%, EAPC 72.82%. On multivariable logistic regression analysis, patients with neoplasms (OR 0.07, p = <0.001) were associated with a lower rate of minimally invasive nephrectomy. Patients with Medicaid (OR 2.21 p = 0.043) and treated at a teaching institution (OR 1.95, p = 0.008) were significantly more likely to undergo minimally invasive nephrectomy. Patients treated at an older age (OR 1.07, p = <0.001) and increasing hospital volume (1.01, p = 0.001), were more likely to be treated with minimally invasive nephrectomy.
Conclusions:
In the last decade, there has been a dramatic increase in the use of minimally invasive nephrectomy, with open nephrectomy still accounting for over 85% of the nephrectomies being performed. However, treatment disparities still exist. Younger patients with neoplasms and private/Medicare insurance, treated at smaller, non-teaching facilities, were less likely to receive minimally invasive nephrectomy. These treatment disparities should be understood, in effort to broaden the availability of minimally invasive nephrectomy in appropriately selected pediatric patients.
Back to Fall Congress
|