|
Back to Fall Congress
A Comparison of the Monti and Spiral Monti Procedure
Benjamin Whittam, MD, Konrad Szymanski, MD, Chandra Flack, BS, Ali Keenan, MD, Rosalia Misseria, MD, Martin Kaefer, MD, Richard Rink, MD, Mark Cain, MD.
Riley Hospital for Children at IU Health, Indianapolis, IN, USA.
A Comparison of the Monti and Spiral Monti Procedures
Background
The Monti technique provides an excellent substitution for the appendicovesicostomy. The spiral Monti is a useful modification to create a long channel when needed. We previously reported outcomes in a large group of patients undergoing Monti and spiral Monti (J Urology, 2007). With short-term analysis there a trend toward increased subfascial revision in the patients with the longer spiral Monti, particularly in those patients with an umbilical stoma. We hypothesized that with longer follow-up the spiral Monti would require more subfascial revisions due to the longer channel length.
Materials & Methods
A retrospective chart review was performed for all patients undergoing the Monti or spiral Monti procedure at our institution. Patient demographics, bowel segment used, stomal location, channel or stoma revisions, number of endoscopic procedures performed, and indications for revision were reviewed. Kaplan-Meier analysis and Cox proportional hazards modeling was used for analysis
Results
Of the 281 patients identified, 138 had Monti procedures and 143 had spiral Monti procedures. Average age at surgery was 10.6 years with an average follow-up of 7.2 years. A total of 87 revisions were performed in 74 patients (26.2%). Of these, 56 were subfascial revisions in 47 patients (16.7%). Subfasical revision rates were 1.9% and 3.3 % per patient year for the Monti and spiral Monti respectively; this difference was not statistically significant (p=0.11).
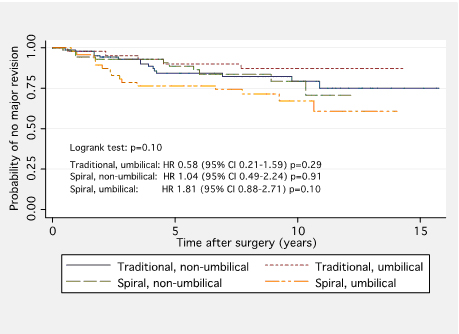
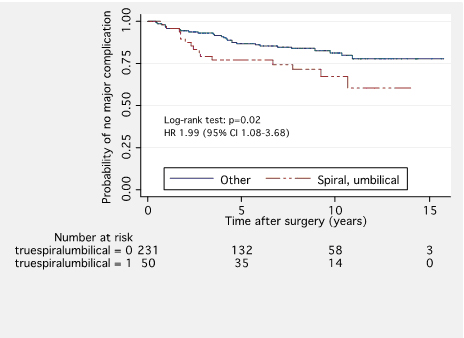
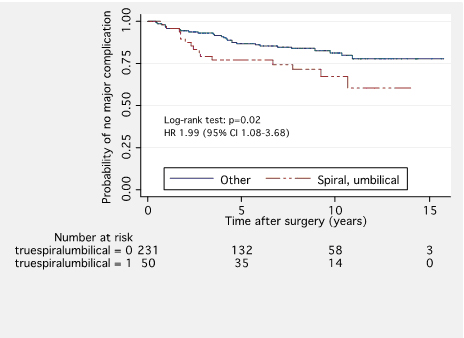
Although no significant difference was identified when patients were further stratified by stomal location (umbilical versus non-umbilical) (p = 0.10), the umbilical spiral Monti showed a trend toward significance (Table 1, Figure 1). When we compared an umbilical spiral Monti to all other channels, it was associated with a two-fold increase in subfasical revision rates (p = 0.02) (Figure 2).
Table 1. | | | Channel : Location | Rate of subfasical revision per patient year (95% CI) | | Monti : Non-umbilical | 2.3% (1.4 – 3.8%) | | Monti : Umbilical | 1.3% (0.5 – 3.2%) | | Spiral Monti : Non-umbilical | 2.6% (1.5 - 4.6%) | | Spiral Monti : Umblical | 4.2% (2.6 – 7.1%) |
Conclusions
We report durable and reliable long-term results with Monti and spiral Monti procedure based on a large patient cohort. There was no significant difference between the Monti and spiral Monti with regard to subfascial revision rates. However, on subgroup analysis, the umbilical spiral Monti was nearly twice as likely
to require a subfascial revision. This finding emphasizes the importance of a well-supported channel with a minimal extravesical component.
Figure 1. Survival Analysis: Monti vs. Spiral Monti
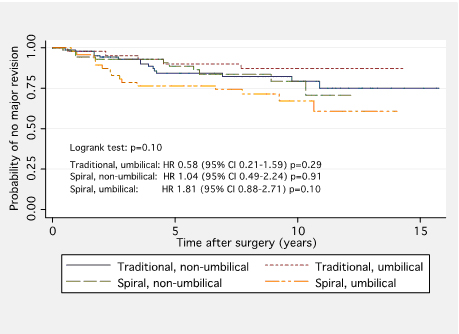
Figure 2. Survival Analysis: Umbilical Spiral Monti vs. All Others
Back to Fall Congress
|