|
Back to Fall Congress
The impact of circumcision status on yield of diagnostic imaging among boys with history of UTI
Caleb P. Nelson, MD MPH, Anthony J. Schaeffer, MD, Emilie K. Johnson, MD MPH, Ilina Rosoklija, MPH, Jeanne S. Chow, MD, Tanya Logvinenko, PhD.
Boston Children's Hospital, Boston, MA, USA.
BACKGROUND:
Imaging after febrile urinary tract infection (UTI) is recommended for both boys and girls. Furthermore, circumcision is thought to be a modifiable risk factor for UTI in boys. However, few data exist comparing the yield of renal/bladder ultrasound (RBUS) and voiding cystourethrogram (VCUG) in circumcised boys versus uncircumcised boys with a history of UTI. We sought to determine whether imaging findings vary by circumcision status in boys undergoing imaging after UTI.
METHODS:
We analyzed RBUS and VCUG findings for 2 groups of male patients who underwent both studies on the same date between 1/1/06-12/31/10. Group A included males 0-60 months with a history of UTI. Group B included males 2-24 months imaged after a first febrile UTI. Patients with any prior postnatal genitourinary imaging or history of prenatal hydronephrosis were excluded. Circumcision status was assessed from the medical record. RBUS and VCUG results were reviewed and classified. Nonparametric descriptive statistics were used to compare RBUS and VCUG findings between circumcised and uncircumcised boys.
RESULTS:
Circumcision status was determined in 356/472 (75%) Group A males (14% were circumcised and 86% were uncircumcised) and in 246/291 (85%) Group B males (15% were circumcised and 85% were uncircumcised).
Ultrasound Findings: For Group A, the proportion of boys with any abnormalities on RBUS (renal/ureteral dilation or renal parenchymal or bladder abnormalities) was 13/50 (26%) among circumcised and 98/306 (32%) among uncircumcised boys (p=0.51). The proportion with moderate or greater hydronephrosis was 1/50 (2%) among circumcised and 10/306 (3.3%) among uncircumcised boys (p=.99). (For reference, 24/1,787 (1.3%) females 0-60 months had moderate or greater hydronephrosis.) Findings were similar for Group B.
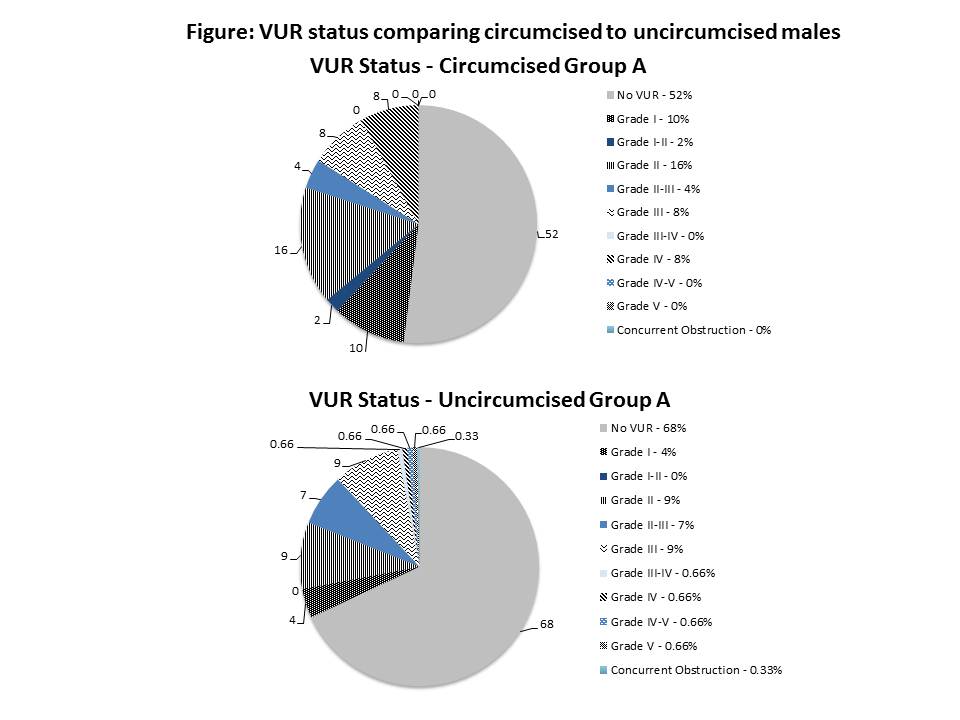
VCUG Findings: In contrast, the findings on VCUG did vary by circumcision status. Vesicoureteral Reflux (VUR) of any grade was identified in 24/50 (48%) circumcised and 97/306 (32%) uncircumcised Group A boys (p=0.04), and in 20/37 (54%) circumcised and 70/209 (33%) uncircumcised Group B boys (p=0.03). (For reference, 803/1,787 (45%) females 0-60 months had VUR of any grade.) High-grade VUR (Grade > III) was identified in 4/50 (8%) circumcised and 8/305 (3%) uncircumcised Group A boys (p=0.07), and in 3/37 (8%) circumcised and 3/209 (1.4%) uncircumcised Group B boys (p=0.045). (For reference, 48/1787 (3%) females 0-60 months had high-grade VUR). The figure shows VUR status stratified by circumcision status for Group A.
CONCLUSIONS:
RBUS findings did not differ significantly between circumcised and uncircumcised boys with a history of UTI, but VCUG findings did vary significantly. Compared to circumcised boys, uncircumcised boys were less likely to have VUR, and when present it was less likely to be high-grade. The lower prevalence of VUR among uncircumcised boys with UTI may be related to the effect of the intact prepuce on UTI risk. Circumcision status could help inform which boys should undergo imaging evaluation after UTI.
Back to Fall Congress
|

