|
Back to Fall Congress
Laparoscopic Varicocelectomy: A single surgeon's experience with over 500 cases
Kenneth I. Glassberg, MD, Scarlett Tohme, BA, Angela M. Fast, MD, Shannon N. Nees, MD, Jason P. Van Batavia, MD.
Division of Pediatric Urology, Morgan Stanley Children's Hospital of New York-Presbyterian Hospital,, New York, NY, USA.
BACKGROUND: Laparoscopic varicocelectomy (LV) has grown increasingly popular for pediatric urologists. Previous reports comparing lymphatic vs non-lymphatic sparing and artery vs non-artery sparing have variable results. We sought to investigate the outcomes of LV in a large cohort of adolescents to determine any differences in outcomes between non-lymphatic sparing, lymphatic sparing and lymphatic and artery sparing procedures as regards post-varicocelectomy hydrocelectomies, recurrences and catch-up growth.
METHODS: 437 patients underwent 534 primary LV (97 bilateral) between 1997 and 2013 (mean age 16yrs). Indications for unilateral vs. bilateral varicocelectomy varied over the 15 years with more done early in the series and much fewer in the last 5 years. 475 varicoceles in 389 patients had at least one follow-up visit at ≥6months post-op (mean follow-up 32months) and the incidence of post-op redo varicocelectomy and hydrocelectomy was determined. Testicular symmetry was calculated by the equation [(right testis volume−left testis volume)/right testis volume]×100 and a cutoff of ≥15% was used for testicular asymmetry. Catch-up growth (CUG) was defined as <15% asymmetry at most recent follow-up visit.
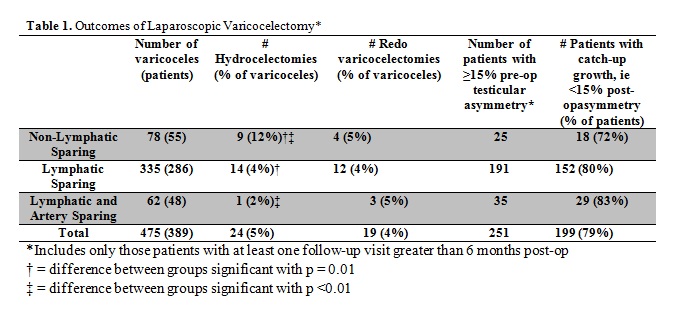
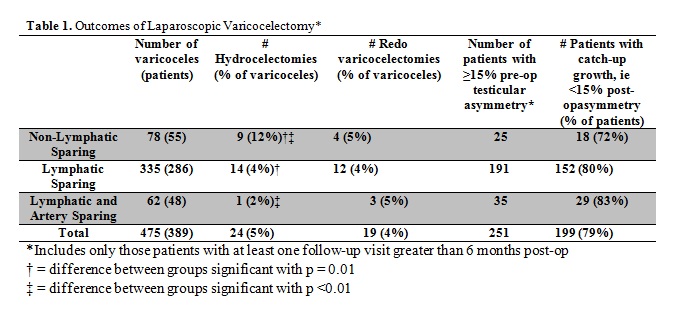
RESULTS: Outcomes based on initial type of laparoscopic varicocelectomy are shown in Table 1. The rate of hydrocelectomy was significantly lower in lymphatic sparing vs. non-lymphatic sparing procedures (p=0.01). All 24 hydrocelectomies were successful. Overall redo-varicocelectomy was performed in 19 patients (4%) and recommended in 5 others who subsequently went elsewhere for care for an overall recurrent varicocele rate of 4.5%. There were no significant differences in varicocele recurrence or redo-varicocelectomy rates between the three procedure groups, although there was a trend for higher recurrence rate in the artery sparing technique vs. non-artery sparing (10% vs. 4%, respectively). All 19 redo-varicocelectomies were successful and thus overall success rate approached 100%. 250 patients had testicular asymmetry at final pre-operative visit and at least one follow-up ultrasound study. Although there was a trend towards more CUG in the lymphatic and lymphatic/artery sparing groups compared with the non-lymphatic group (80% and 83% vs. 72%, respectively) this difference was not significant.
CONCLUSIONS: All 3 LV procedures offer similar success and CUG rates in boys. While varicocele recurrence occurs in 4.5% of boys regardless of laparoscopic technique, all redo procedures were successful. Artery-sparing offers no significant benefit as regards CUG. While lymphatic-sparing varicocelectomy is beneficial in decreasing the rate of post-operative hydroceles, it does not increase the recurrence rate. Overall success rate, including redo procedures, approached 100%. Considering the facts that the initial laparoscopic repair ignored possible collateral vessels distal to the internal inguinal ring, of the 19 redo-varicocelectomies only one deferential and one external spermatic vein were ligated, and that no testicle was mobilized into the operative field leads us to question the importance of collaterals below the level of the internal ring. Specifically, these findings question the role that scrotal collaterals play in the original formation of the varicocele and the reason for recurrence.
Back to Fall Congress
|