|
Back to Fall Congress
Cutting for stone in augmented bladders: What is the risk of recurrence and is it impacted by treatment modality?
Konrad M. Szymanski, MD MPH, Rosalia Misseri, MD, Benjamin Whittam, MD, Sable Amstutz, BSc, Martin Kaefer, MD, Richard C. Rink, MD, Mark P. Cain, MD.
Riley Hospital for Children, Indianapolis, IN, USA.
BACKGROUND:
Bladder stones are common after bladder augmentation, resulting in numerous procedures for recurrent stone removal over the course of a patient’s lifetime. In addition, it has been suggested that stone recurrence may be lower if stones are treated without fragmentation to minimize residual stone nidus. We aimed to quantify stone recurrence in augmented bladders and determine risk factors.
METHODS:
We conducted an IRB-approved, retrospective review of 108 patients treated for a first bladder stone at our institution. Patient demographics, prior surgeries, mode of bladder stone therapy and recurrences were reviewed. Kaplan-Meier analysis and Cox proportional hazards modeling was used for analysis.
RESULTS:
Of 108 patients, 59 (54.6%) were female, 86 (79.5%) had neuropathic bladder (myelomeningocele, sacral agenesis, lipomeningocele, spinal dysraphism, cerebral palsy) and 56 (51.9%) used a wheelchair. Children were augmented at a mean of 8.9 years old and followed for a mean of 8.8 years (range 4mo.-25.7 years). Segments used for augmentation included ileum (72.2%), sigmoid (16.7%), cecum/ileocecum (9.3%), ureter (0.9%) and stomach/ileum (0.9%) with a catherizable channel in 82 (75.9%). A bladder neck procedure was performed in 68 (63.0%) (reconstruction: 38.0%, sling: 16.7%, AUS: 6.5%, closure: 1.9%). Recurrent UTIs with urea splitting organisms were noted in 18.5%. First stone surgery occurred 3.6 years post-augmentation (median, range 4 months-21.8 years). Endoscopy was used in 67.6%, open cystolithotomy in 32.4%. While 48.2% of stones were fragmented, 51.9% were not. 42.6% of first stones were struvite.
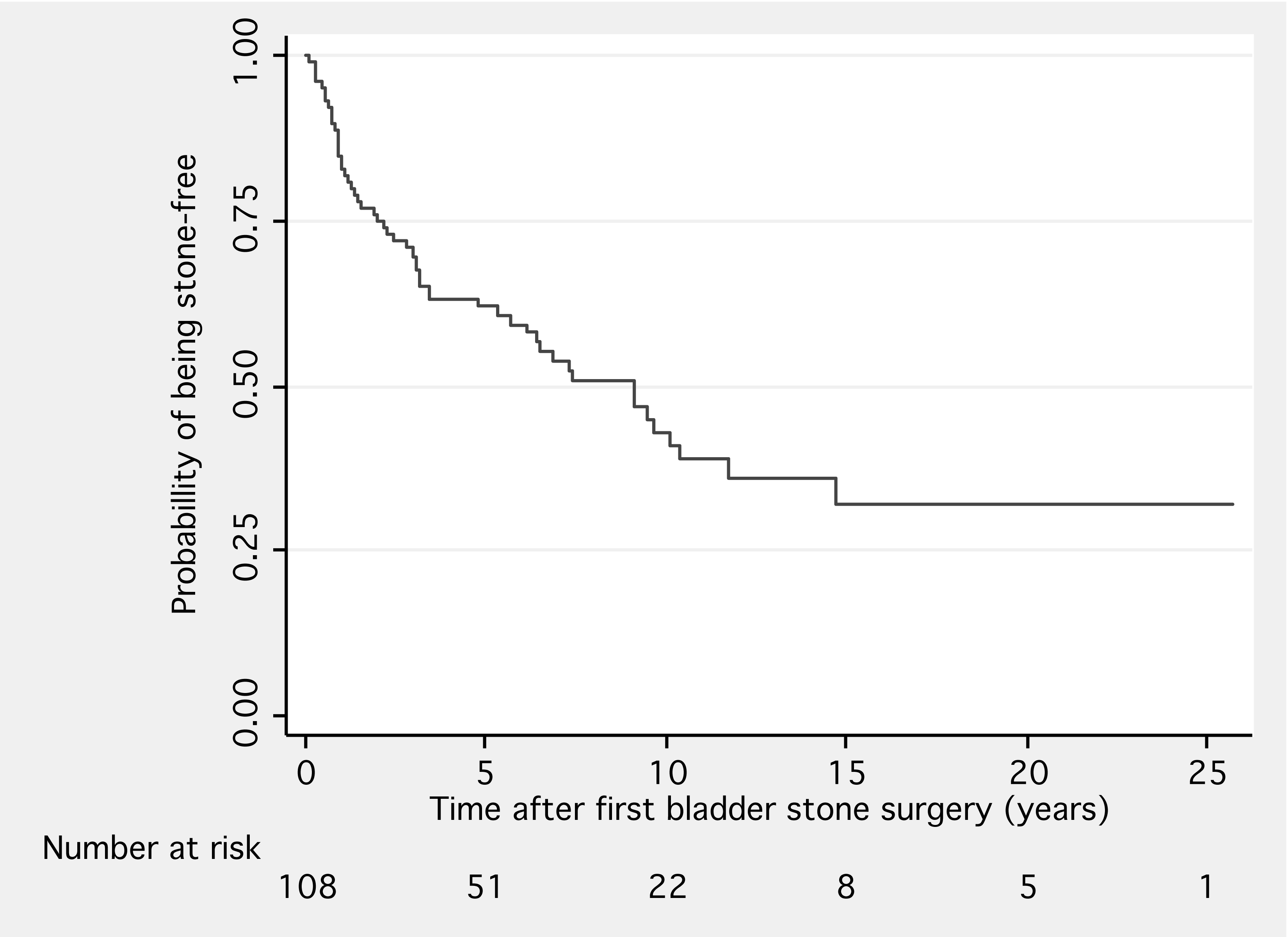
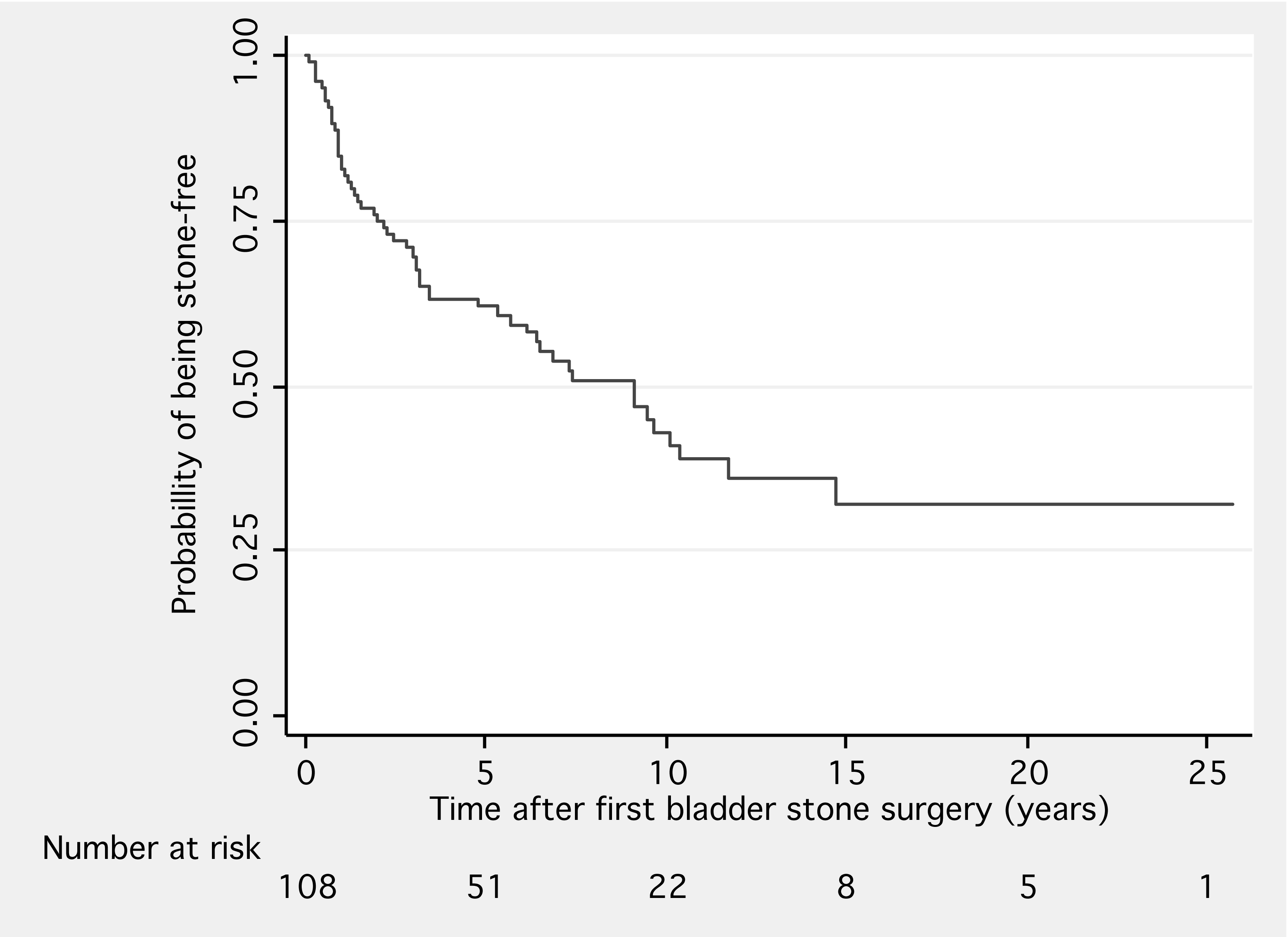
Stones recurred in 54 (50.0%) patients, requiring a mean of 2 surgeries for recurrences (range 1-10). Median recurrence time was 9.1 years (range 1mo.-14.7 years) (Figure 1). Overall, the recurrence risk was 8.4% per patient per year (95% CI 6.4-11.0%) and remained elevated over the first 10 years of follow-up. Annual risk appeared highest within the fist 4 years: 13.9% per patient per year 1 and year 2, as well as 9.5% per patient per year 3-4.
Recurrence risk did not change whether the first stone was treated by open or endoscopic technique, with or without fragmentation, even after controlling for immobility, segment used, presence of catherizable channel, bladder neck surgery, history of nephrolithiasis, recurrent UTIs or stone composition on multivariate analysis. This persisted even after correcting for date of surgery, patient age or early recurrence on exploratory analysis.
CONCLUSIONS:
Bladder stones recurred in half of patients at 9 years, independent of treatment technique and patient characteristics. Being a high risk group, these patients require mandatory annual US and KUB films. Given an annual recurrence risk of 10% or higher within 4 years after the first stone event, we suggest an annual cystoscopy in the clinic for possible removal of small stones and augment surveillance.
Back to Fall Congress
|