|
Back to Fall Congress
Impact Of Pediatric Multidisciplinary Stone Clinic On Urinary Risk Parameters In Stone-Forming Children
Adam J.M. Kern, M.D., Bhavik B. Shah, M.D., Gautam Jayram, M.D., Heather N. DiCarlo, M.D., Eric Z. Massanyi, M.D., John P. Gearhart, M.D., Alicia Neu, M.D., Brian R. Matlaga, M.D., M.P.H..
Johns Hopkins, Baltimore, MD, USA.
BACKGROUND:
Utilization of a multidisciplinary stone clinic (MSC) has been shown to significantly improve urinary parameters and stone recurrence rates in the adult population. The goal of the current study was to assess the impact of MSC on urinary parameters in a population of stone-forming children. Additionally, we sought to identify whether dietary management alone in the context of the multidisciplinary clinic is sufficient to resolve abnormal urine parameters.
METHODS:
A retrospective cohort study of patients treated in our pediatric multidisciplinary stone clinic between January 2006 and July 2012 was performed. Patients’ urinary stone risk factors were evaluated with baseline 24-hour urine collections. Following appropriate dietary or medical intervention, patients underwent follow-up 24-hour urine analyses and the results were assessed. Duration and type of therapy were included in the analysis. The primary endpoint was improvement in urinary stone risk factors as a function of participation in MSC. Secondary endpoints were improvement in urinary stone risk factors following dietary- or medical-specific intervention.
RESULTS:
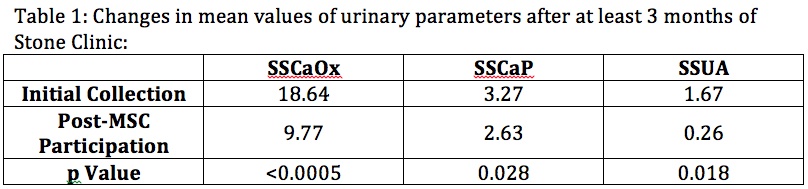
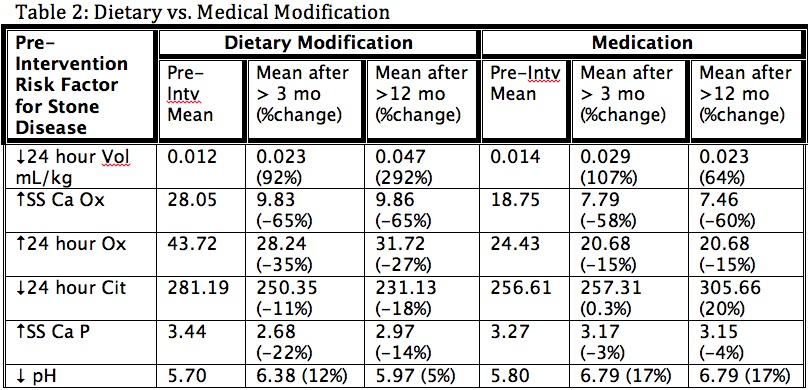
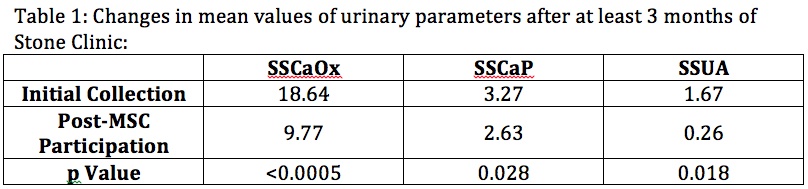
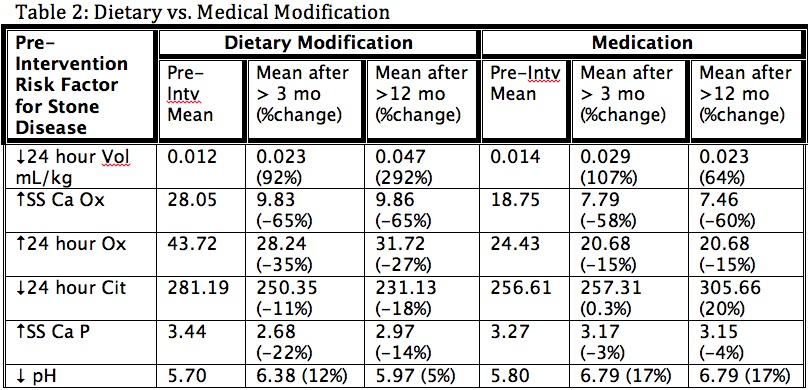
Thirty-one subjects who underwent 111 discrete 24-hour urine collection studies were identified. Mean follow-up for this group was 1.96 years. Twelve (39%) patients had symptomatic stone events during the follow-up period. Following participation in the dedicated pediatric MSC, subjects exhibited significant improvements in urine volume (0.014 vs. 0.025 L/kg/day; p<0.043), 24-hour oxalate (48.93 vs. 30.59 mg/day; p<0.0038), and urinary pH (5.70 vs. 6.46; p<0.013). Additionally, subjects showed a significant and durable reduction in 24-hour urinary calcium excretion (341.38 vs. 154.37 mg/day; p<0.044) after at least 12 months of follow-up. Improvements in supersaturations of calcium oxalate (SSCaOx), calcium phosphate (SSCaP), and uric acid (SSUA) are depicted in Table 1. Table 2 compares the impact of dietary vs. medical therapy on 24 hour urine volume, SSCaOx, 24 hour Ox, 24 hour citrate, SS Ca P, and urine pH. Time-dependent improvements in urinary parameters with dietary vs. medical management are depicted in Table 2.
CONCLUSIONS:
We observed a significant and beneficial impact of a dedicated pediatric MSC on measured urinary stone risk parameters. Furthermore, patients with prolonged follow-up and surveillance in the MSC appear to derive continued benefit. For certain types of stone formers dietary management as monotherapy may be effective. Our analysis also suggests values for expected minimum duration of therapy prior to resolution of urine stone risk parameters. Taken all together, our findings support the use of a MSC as an ideal management strategy in the management of pediatric urolithiasis.
Back to Fall Congress
|