|
Back to Fall Congress
National Trends in Surgery for Vesicoureteral Reflux
Curtis Clark, MD1, Rhys Irvine, MD1, Benjamin Chung, MD2, Steven Chang, MD3.
1Childrens Hospital Medical Center of Akron, Akron, OH, USA, 2Stanford University Medical Center, Stanford, CA, USA, 3Brigham and Women's Hospital, Boston, MA, USA.
National Trends in Surgery for Vesicoureteral Reflux
Background:
In recent years the advent of endoscopic and minimally invasive surgery for vesicoureteral reflux (VUR) and evolving knowledge of the relationship between VUR, urinary tract infection, renal scarring, and dysfunctional elimination has impacted the frequency and type of interventions performed. Furthermore, practice patterns have changed to eliminate the routine correction of VUR when persistent beyond 5-6 years of age. We sought to evaluate contemporary national trends in the numbers and types of surgery for VUR in the United States.
Methods:
We conducted a retrospective cohort study of pediatric patients (≤18 years) who underwent ureteroneocystostomy (UNC, ICD9 56.74) or endoscopic surgery for VUR (ICD9 57.32) between January 1, 2003, and December 31, 2010, from the Premier Perspective database (Premier Inc, Charlotte, NC), which includes a 20% sample of US hospital discharges. Patients were confirmed to have undergone endoscopic surgery by identifying associated billing codes containing the words “Deflux.” Descriptive statistics with least squares regression and chi-square analysis were used to characterize our study population accounting for survey weighting to yield a nationally representative result. We determined the annual number of surgeries, unilateral/bilateral UNC, number of procedures per patient, and whether patients underwent both types of surgery. The use of minimally invasive UNC (i.e., laparoscopic or robotic) was determined through a review of the billing record for each patient.
Results:
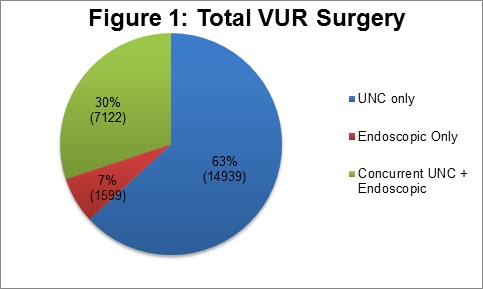
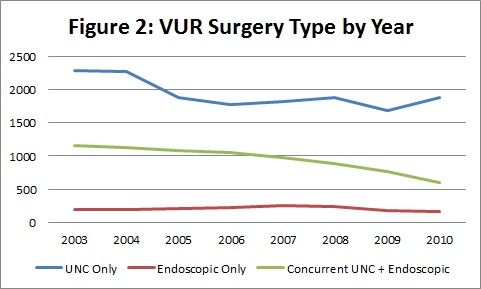
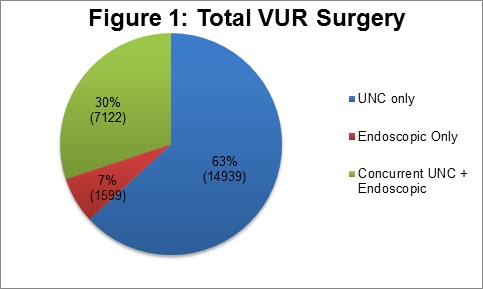
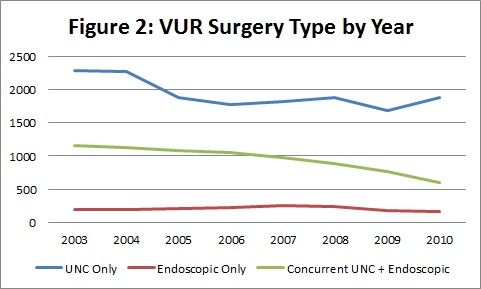
The study cohort included 3,911 patients equaling a weighted sample size of 23,660 patients. During the study period, UNC was the predominant form of surgical therapy (Figure 1). Unilateral UNC was consistently more common than bilateral UNC by a ratio of 4:1, while laparoscopic (3%) and robotic (1.2%) approaches were uncommon. The annual number of VUR surgeries progressively decreased by nearly 4% annually, which was driven primarily by the reduction in UNC. Approximately 37% of all patients underwent endoscopic therapy, and the majority of these patients (80%) received endoscopic therapy in the setting of a concurrent UNC (Figure 2). Fewer than 3% of patients underwent subsequent repeat procedures for VUR during the studied period.
Conclusion:
There is a contemporary trend for decreasing use of surgery in the management of VUR. Open UNC remains the mainstay of surgical treatment despite advances in minimally invasive and endoscopic techniques. Endoscopic therapy was mainly employed in concert with UNC, potentially as an adjuvant treatment to minimize the risk of post-operative contralateral VUR or to avoid bilateral extravesical UNC. Limitations include the failure to capture surgery (primarily endoscopic) which may be performed in an outpatient surgery center, as well as the possibility that the database sample fails to accurately represent pediatric hospitals. Further study is necessary to determine whether our observed trend continues, reverses, or stabilizes.
Back to Fall Congress
|