|
Back to Fall Congress
Overactive Bladder in Children: Associations with Symptoms and Specific Lower Urinary Tract Conditions
Jason P. Van Batavia, MD, Angela M. Fast, MD, Andrew J. Combs, RPA-C, Kenneth I. Glassberg, MD.
Division of Pediatric Urology, Morgan Stanley Children's Hospital of New York-Presbyterian Hospital,, New York, NY, USA.
BACKGROUND: According to the ICS and ICCS, overactive bladder (OAB) is defined by the subjective symptom of urgency. While no other symptom or any specific urodynamic finding is required for its designation, it is widely presumed to be associated with detrusor overactivity (DO) and often thought to be associated with increased urinary frequency, decreased functional bladder capacity, and urge incontinence. We sought to determine how often these symptoms and findings are associated with urgency in children.
METHODS: We reviewed our database for neurologically/anatomically normal children presenting with urgency. Incidence of frequency, daytime incontinence and percent expected bladder capacity (%EBC; [actual bladder capacity]/[expected bladder capacity]) were recorded. Mean %EBC was compared between urgency alone, associated symptoms and gender. Lastly, we reviewed final LUT condition diagnosis for each child to see how what condition children with OAB ultimately were diagnosed with. LUT conditions included: dysfunctional voiding (DV), idiopathic detrusor overactivity disorder (IDOD), detrusor underutilization disorder (DUD, similar to willful retention), and primary bladder neck dysfunction (PBND). While DO can occur with any LUT condition it is the driving force behind IDOD.
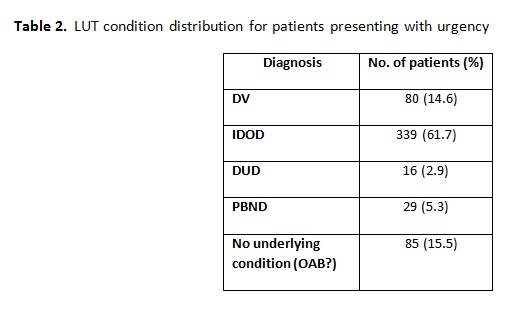
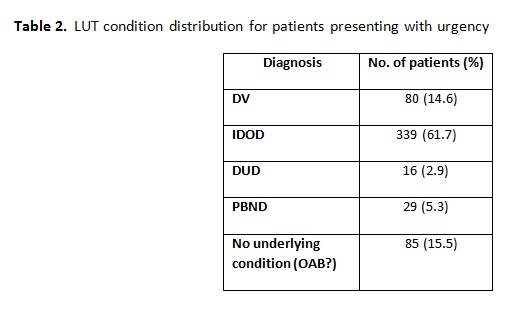
RESULTS: 548 children (231M, 318F; mean age 9.0, range 3-20) presented with urgency. Daytime incontinence was reported in 398 (72.6%) and frequency was reported in 258 (47.1%). Mean %EBC was 80.9. Patients with urgency alone had a normal %EBC, which significantly decreased with each additional LUT symptom (Table 1). When stratifying by gender, females were more likely to report daytime incontinence (76.7% vs. 67.5%, p=0.02) and frequency was found more often in males (63.7% vs. 38.1%, p<0.001). Males also had decreased %EBC compared to females (70.0 vs. 88.8, p<0.001). Table 2 illustrates the final diagnoses in patients presenting with urgency. While the majority were ultimately diagnosed with IDOD, almost 15% of children who fall under the category of OAB were diagnosed with DV and another 5% with PBND.
CONCLUSIONS: Urgency alone (ie OAB) was indeed commonly associated with daytime incontinence, but not to the universal degree often presumed. The incidence of OAB was greater in females who tended to have less frequency and better %EBC but were more likely to wet. Conversely, males tended to have more frequency and lower %EBC but were less likely to wet, possibly reflecting better holding maneuvers resulting in thicker, more muscular, less compliant bladders. Children who present with urgency (ie, OAB) will ultimately be diagnosed with a variety of LUT conditions all of which are distinct entities and require specific individualized treatment.

Back to Fall Congress
|