24-hour Urine in Pediatric Stone Patients: Does positive family history predict metabolic abnormalities?
Derrick Johnston, MD1, Elizabeth Tourville, MD1, Sean Corbett, MD2, George Chiang, MD3, Gina Gina Cambareri, MD4, Rhys Irvine, MD1, Aaron Bayne, MD5, Larisa Kovacevic, MD6, Dana Giel, MD1.
1University of Tennesse, Memphis, TN, USA, 2University of Virgina, Charlotteville, VA, USA, 3Rady Children's Hospital, San Diego, CA, USA, 4Beth Israel Medical Center, Newark, NJ, USA, 5Oregon Health & Science University Hospitals, Clackamas, OR, USA, 6Children's Hospital of Michigan, Detriot, MI, USA.
Introduction: The burden of pediatric stone disease is increasing over time. Current literature provides evidence of familial and genetic influences on pediatric stone incidence. In this multi-institutional study, we evaluate the hypothesis that pediatric stone patients are more likely to have abnormal 24 hour parameters if they have a positive family history for stone disease.
Methods: 24-hour urine parameters were collected on children with urolithiasis at five institutions from 2000-2013 using a standard assay (LithoLink) and analyzed with respect to family history of stone disease. Statistical analysis was performed in aggregate and stratified by age, BMI, and stone composition. Mann-Whitney U test was performed for continuous variables and Fisher’s Exact Test was used for categorical variables.
Results: 246 children met inclusion criteria. 120 (49%) had a positive family history of stone disease. 232 (94%) had at least one abnormality on 24−hour urine analysis. No statistically significant correlation was noted between family history and any of the 24-hour electrolytes included in the assay either in mg/day or after adjusting by weight or body surface area. The supersaturation ratios of calcium oxalate and calcium phosphate showed no correlation with family history. There was a trend towards increased uric acid supersaturation in children with a positive family history, but this did not meet statistical significance (p = .072). No new correlation resulted after stratifying by age, BMI, or stone composition.
Conclusion: Analysis of the data in this multi-institutional study does not support the hypothesis that family history increases risk of 24-hour urine abnormalities among children who have already been diagnosed with stone disease. There is a high rate of 24-hour urine abnormalities in all children with urolithiasis regardless of family history. The presence or absence of family history should not influence the decision to perform 24-hour urine studies for children with stone disease. 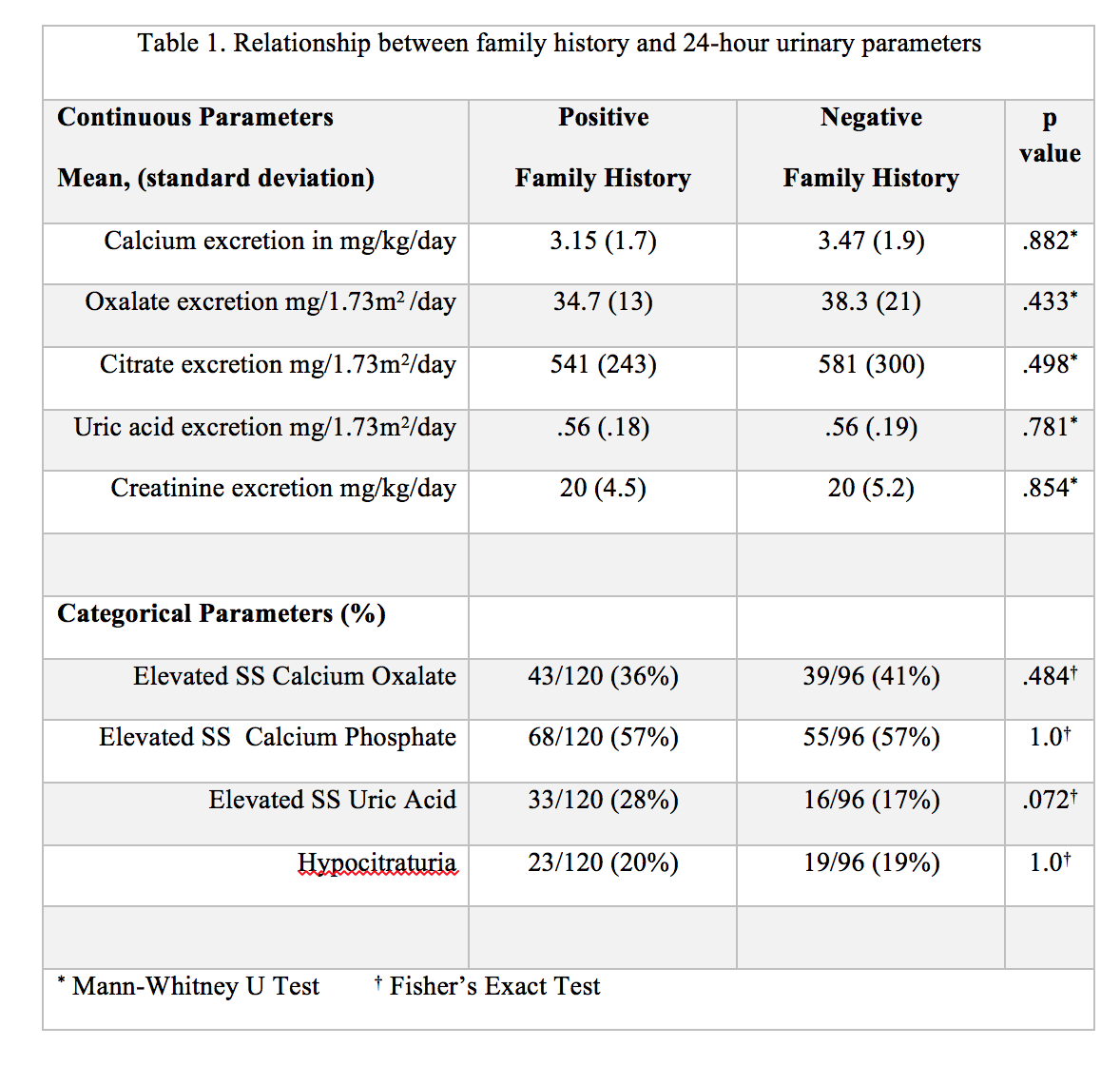
Back to 2016 Fall Congress
