Dietary modification and education positively affects 24-hour urine chemistry in pediatric urolithiasis
Michael K. Lam, MD1, Amanda G. VanDlac, MD1, Dana Giel, MD2, Larisa G. Kovacevic, MD3, Sean T. Corbett, MD4, George Chiang, MD5, Gina M. Cambrareri, MD6, Aaron P. Bayne, MD1.
1Oregon Health & Science University, Portland, OR, USA, 2University of Tennessee Health Science Center, Memphis, TN, USA, 3Children's Hospital of Michigan, Detroit, MI, USA, 4University of Virginia Health System, Charlottesville, VA, USA, 5Rady Children's Hospital, San Diego, CA, USA, 6Children’s Hospital of New Jersey at Newark Beth Israel Medical Center, Edison, NJ, USA.
Background
Nephrolithiasis in the pediatric population has long been associated with a high recurrence rate. Many have identifiable metabolic risk factors, which if targeted may help reduce their risk of recurrence. 24-hour urine chemistry has been a useful tool in the adult population to help identify these risks, which then aids the physician in patient education as well as treatment. It is unclear whether dietary modification in pediatric patients has impactful clinical differences. Here we undertook a study to determine whether therapies of dietary education, hydrochlorothiazide (HCTZ), or potassium citrate can affect 24-hour urine parameters in children.
Methods
We performed a multi-institutional retrospective study to identify patients aged 2-18 who received dietary education, HCTZ, or potassium citrate from 2006-2013. Patients were included if they performed 24-hour urine collections prior to and after treatment. We compared changes in 24-hour urine parameters across each cohort.
Results
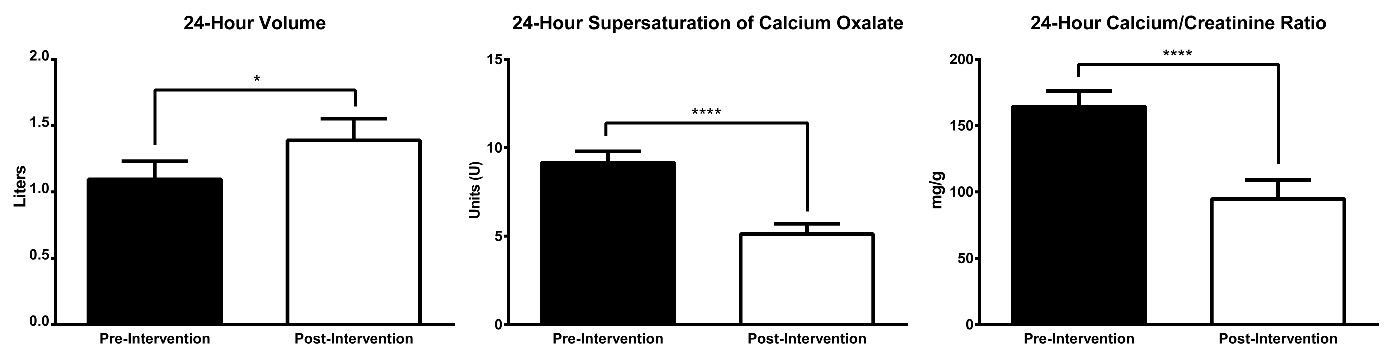
80 patients in total were identified. 60 (66.7%) were treated with dietary changes and education, 9 (10.0%) were treated with hydrochlorothiazide, and 21 (23.3%) were treated with potassium citrate. There were no significant differences in gender, age, BMI, or interval time between urine collections. Patients who underwent dietary modification had significant pre and post-treatment differences in 24-hour urine volume (1.2L vs 1.5L, p ≤ 0.01), supersaturation of calcium oxalate (165.3 vs 71.1, p ≤ 0.05), and calcium/creatinine ratios (8.82 vs 3.92, p ≤ 0.05). There were no significant differences in urine parameters of patients who received HCTZ or potassium citrate.
Conclusions
Patient education in the form of dietary modification positively affects metabolic risk factors associated with recurrent stone disease. Future research will continue to examine the efficacy of medical therapies in pediatric nephrolithiasis, as well as whether or not interventions directly reduce stone recurrence. 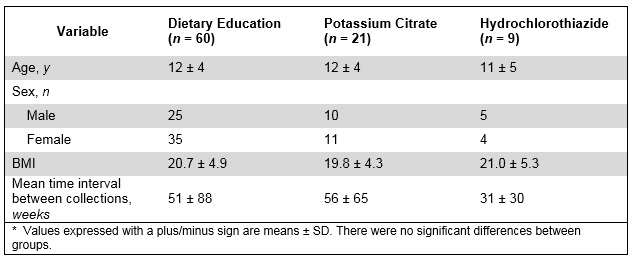
Back to 2016 Fall Congress
