Is there a functional disadvantage to using the external iliac vessels for anastomosis in pediatric and adolescent patients undergoing renal transplantation?
Michele Gnech, MD1, Katherine Taylor, MD2, Martin A. Koyle, MD2, Mandy Rickard, MN-NP1, Luis H. Braga, MD1, Armando J. Lorenzo, MD2.
1McMaster University, Hamilton, ON, Canada, 2University of Toronto/ The Hospital for Sick Children, Toronto, ON, Canada.
Introduction
Renal transplantation (RT) remains the best available strategy for addressing stage 5 chronic kidney disease in children and adolescents. Technical aspects of the procedure can have a clear impact on complications and health of the allograft, including delayed graft function (DGF). Immediate optimal perfusion is paramount, thus choosing a target vessel has to take into account the flow demands imposed by an adult-size kidney in an proportionally smaller recipient. Herein we explore the hypothesis that vascular anastomosis location can impact DGF independent of patient age and size.
Methods
Retrospective review of a single institution referral center transplant database, including data on 156 patients. We collected data on patient characteristics (age, height, body surface area [BSA], gender, preoperative need for dialysis), donor source (deceased vs. living), warm and cold ischemia time (WIT/CIT), hemodynamics during the procedure, use of inotropes or diuretics, and location of the arterial and venous anastomoses. The primary outcome, DGF, was assessed by measuring the time to nadir creatinine (ttNC, in days), dichotomized at 1 week for multivariable logistic regression analysis adjusting for age and BSA.
Results
Location of the arterial anastomosis was clearly impacted by age and donor size (Figure 1A). On univariate analyses longer ttNC was associated with deceased vs. living donor (11.8+/-11.5 and 4.3+/-5.0; p<0.001), preoperative need for dialysis (9.7+/11.0 and 6.5+/-6.0, p=0.02), location of arterial anastomosis (Aorta [n=21] 4.9+/-6.1, common iliac [n=93] 7.1+/-7.3, external iliac 14.7+/-14.5; p<0.001, Figure 1B) and venous anastomosis (Vena Cava [n=21] 5.6+/-6.3, common iliac [n=89] 7.1+/-7.6, external iliac [n=44] 13.8+/-14); p<0.001). On multivariable analysis this association remained statistically significant when adjusting for recipient age, height, BSA, donor source, change in blood pressure with unclamping, use of inotropes and preoperative dialysis. The detrimental effect on ttNC was most robust when comparing external iliac vs common iliac and Aorta or Vena Cava.
Conclusion
Our data suggests that anastomosis to a smaller calibre target vessel (i.e. external iliac) in comparison to the common iliac or Aorta/Vena Cava may be a risk factor for delayed return of graft function, independent of recipient size and donor source. This finding merits further evaluation, as it may help with intraoperative decision making during pediatric and adolescent renal transplantation. 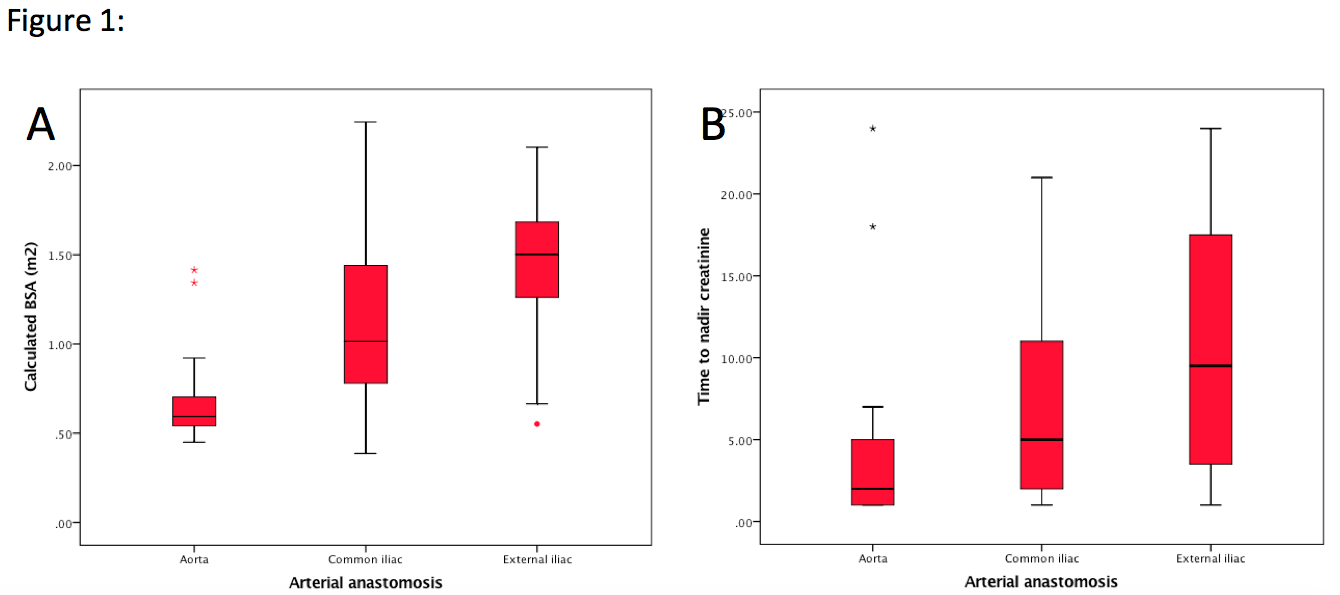
Back to 2016 Fall Congress
