Modulation Of The Rat Micturition Reflex With Transcutaneous Ultrasound
Daniel P. Casella, M.D., Anne G. Dudley, M.D., Douglass B. Clayton, M.D., John C. Pope, IV, M.D., Stacy T. Tanaka, M.D., John Thomas, M.D., Mark C. Adams, M.D., John W. Brock, III, M.D., Charles F. Caskey, PhD.
Vanderbilt Univeristy, Nashville, TN, USA.
Background:
Indirect modulation of the S3 nerve root via peripheral nerve (posterior tibial) stimulation is an effective therapy for overactive bladder and voiding dysfunction. Clinical application of this approach is limited by the need to place a needle electrode, frequency of treatment and the discomfort associated with the stimulator pulses.
Focused high frequency ultrasound has recently been identified as a novel method of neurostimulation in the central nervous system and peripheral nerves. We hypothesized that ultrasound stimulation of the posterior tibial nerve would inhibit bladder contractions in an established model of rhythmic bladder contractions in the anesthetized rat.
Methods:
Experimental Setup:
Under urethane anesthesia, female rats (230-300 grams) were transurethrally catheterized with an 18 gauge angiocatheter. Cyclical detrusor contractions were initiated by infusing saline into the bladder at 0.05mL -0.15ml/min. Once established, the saline infusion was stopped and bladder contractions continued indefinitely. Prior to initiating pulses, the ultrasound probe was positioned superior to the medial malleolus, over the course of the posterior tibial nerve.
Ultrasound Stimulation Protocol: Ultrasound pulses were delivered in time intervals of 5 -10min using a single element spherically focused 250 kHz transducer (62 cycles repeated at 2 kHz for 300 msec at peak negative pressure of 900 kPa pulsed at 0.5 Hz).
Results:
We demonstrate successful suppression of bladder contractions using ultrasound stimulation in 10 animals. Our initial experiments in 6 animals used 5 minutes of ultrasound stimulation. We then increased the duration of ultrasound treatment to 10 minutes in 3 animals and 15 minutes in 1 animal. The average latency between the initiation of ultrasound and suppression of bladder contractions was 3 minutes 23 seconds (+/- 51 seconds), the average time of contraction suppression was 13 minutes and 50 seconds (+/- 2 minutes 25 seconds) and the average time from the end of ultrasound to return of contractions was 9 minutes 37 seconds (+/- 2 minutes and 30). We also successfully suppressed bladder contractions again by reapplication of ultrasound 50 and 70 minutes after the initial stimulation. Application of ultrasound at 15, 20, 30 and 40 minutes after the initial stimulation did not suppress contractions. In contrast to prior studies utilizing electrical stimulation, our ultrasound parameters did not induce a motor response in the rat foot.
Conclusion:
In this work, we demonstrate the ability of transcutaneous ultrasound mediated posterior tibial nerve stimulation to inhibit rhythmic bladder contractions in anesthetized rats. When compared to direct electrical stimulation, ultrasound stimulation delivers energy at a lower frequency. Given that pain sensation directly correlates with the frequency of the stimulus, ultrasound mediated tibial nerve stimulation may reduce discomfort. Due to its non-invasive nature and ease of application, we believe ultrasound mediated tibial nerve stimulation is potentially an ideal outpatient treatment of overactive bladder and dysfunctional elimination. 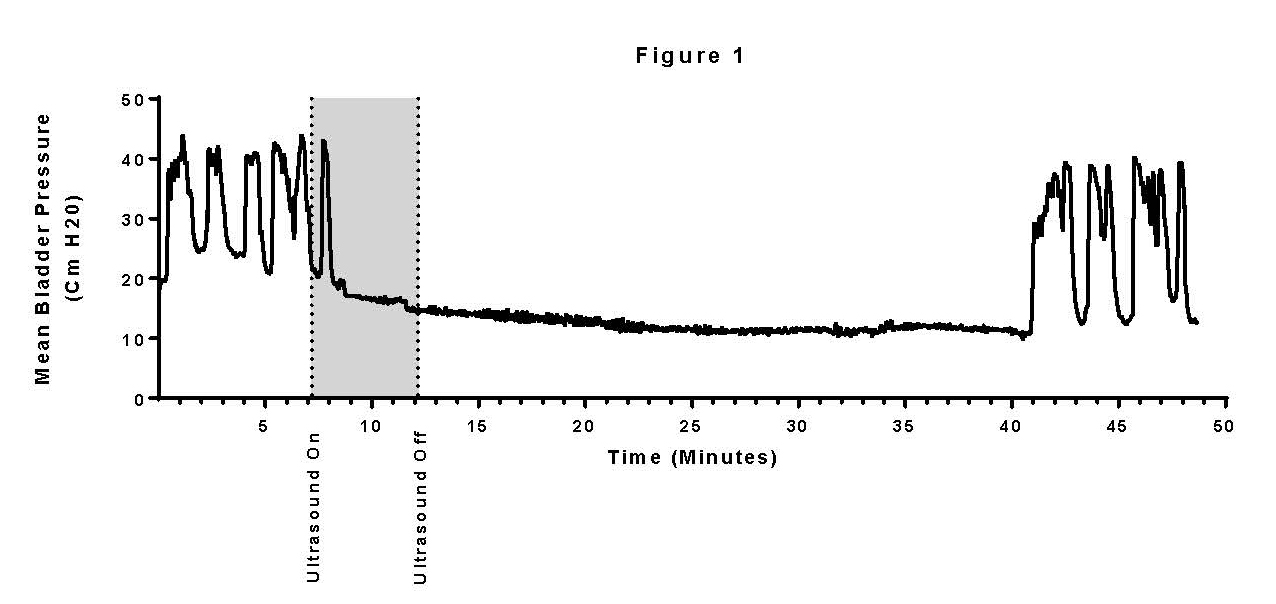
Back to 2016 Fall Congress
