The modified Ulaanbaatar procedure: reduced complications and enhanced cosmetic outcome for the most severe cases of hypospadias
Venkata R. Jayanthi, MD, Christina B. Ching, MD, Daniel G. DaJusta, MD, Daryl J. McLeod, MD, Seth A. Alpert, MD.
Nationwide Children's Hospital, Columbus, OH, USA.
The modified Ulaanbaatar procedure: reduced complications and enhanced cosmetic outcome for the most severe cases of hypospadias
Introduction:
The “Ulaanbaatar” procedure for proximal hypospadias was described by Dewan as a modification of the classic 2-stage procedure in which the glanular urethra is constructed during the first stage. During the second stage, the penile skin between native proximal meatus and the distal reconstructed urethra is tubularized, as in a Johanson urethroplasty.
Materials and Methods:
We retrospectively reviewed all consecutive patients who completed both stages of the repair. We evaluated demographics, original meatal location, technique of chordee correction, technique of glanular urethra reconstruction and overall outcomes and complications. The first stage is analogous to a classic repair with regard to urethral plate division and chordee correction (plication vs ventral grafting). Our modification involves creation of a preputial tubularized island flap which is brought through the glans. The remaining penile skin is used for skin coverage and to bridge the native meatus and the distal neourethra. Six months later, the midline skin is tubularized reconstructing the urethra from the proximal meatus to the glanular neourethra constructed at the first stage.
Results:
Thirty-three boys have undergone both stages. Mean age at surgery was 18.3 months (range 6-118). Initial urethral meatal location was mid-scrotal in 26 (79%), perineal in 6 (18%) and coronal in 1 (3%). Nineteen underwent evaluation for genital ambiguity at birth (58%). Twenty-nine (88%) received pre-operative testosterone or HCG. After urethral plate transection, persistent curvature was addressed during the first stage with dorsal plication in 12 (36%), urethral plate transection alone in 6 (18%) or ventral grafting with small intestinal submucosa (SIS) in 15 (46%). Twenty-two (67%) had the neourethra tunneled through the glans and 11 (33%) had the glans split followed by glanuloplasty. Average time between the two stages was 7 months (range 4.0 - 13.9 months). Bifid scrotum/penoscrotal transposition was corrected at the first stage in 3 and at the second in 22. Three patients (9%) developed urethral diverticula that required repair. One developed recurrent epididymitis related to an abnormal ejaculatory duct (no stricture) and underwent vasectomy. No patient developed a fistula. Mean length of follow up is 15.2 months (0.3 to 50.2).
Conclusions:
Our modification involves the formation of a tubularized island flap of preputial skin to create the distal urethra during the first stage. The second stage is relatively simple as it is analogous to a large fistula repair. This technique may improve the cosmetic appearance as the glans is only touched once and it may permit a “tunneled” glanular urethra. Its use is applicable to the most severe cases of hypospadias where urethral plate transection is necessary, particularly those with genital ambiguity. 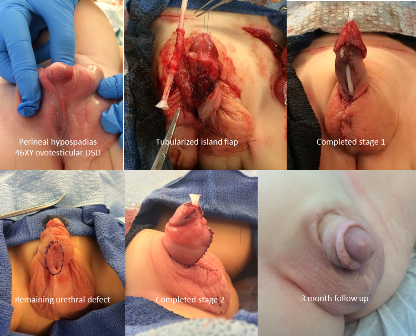
Back to 2016 Fall Congress
