Reassessing the Utility of Routine Urine Culture with Urodynamics: UTI Incidence and Risk Factors
Devon C. Snow-Lisy, MD, Christopher Halline, BS, Emilie J. Johnson, MD MPH, Dawn Diaz-Saldano, APN, NP, Theresa Meyer, RN, MS, CPN, Elizabeth B. Yerkes, MD.
Ann and Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, USA.
BACKGROUND: There is currently no consensus regarding the need for peri-procedural antibiotics or routine urine cultures during urodynamics (UDS) in children. At our institution we historically have obtained urine cultures during UDS. However, even in the setting of a positive culture we have observed that only a minority of patients require treatment. Most are successfully managed with increased hydration and increased frequency of bladder emptying. The aim of this study was to evaluate clinical characteristics, treatment rates, and outcomes in patients undergoing UDS in order to identify risk factors for UTI, and identify who may benefit from routine urine culture.
METHODS: This study was a retrospective review of 600 patients who underwent 807 UDS between 1/2013-1/2015. Positive urine culture was defined as >104 colony forming units /ml. Afebrile UTI was defined as the presence of new symptoms within 7 days. Febrile UTI was the above + fever > 38.5◦C. Fisher’s exact test was used for categorical comparative analysis.
RESULTS: Patients were 6.9 years old (median) at the time of UDS (Range 0.1-25.2, IQR 2.7-12.4). Males represented almost half of the cohort (47%, 282/600). Common diagnoses were neurogenic bladder in 47% (282/600), hydronephrosis in 44% (262/600), vesicoureteral reflux in 22% (130/600), and bladder dysfunction in 20% (117/600). Patients were on antibiotics 22% of the time prior to UDS (prophylactic dose 157/807, therapeutic dose 21/807). The majority of patients had a urine culture taken immediately prior to UDS (765/807; 94.8%). Patients on clean intermittent catheterization (CIC) were more likely to be on antibiotics prior to the procedure, 26.1% (95/362) vs. 18.4% (81/440) respectively (p=0.02). Positive culture was seen in 46.0% (352/766) with significantly more positive cultures in patients on CIC versus no CIC (78.2% (275/352) vs. 21.8% 77/352, p< 0.0001). Clinical UTI within 30 days prior to UDS was predictive for UTI and/or need for treatment (Table 1, p=0.04). Twelve patients (1.5%, 95% Confidence Interval 0.66-2.34%) developed a UTI, 41.7% (5/12) of which were febrile with none requiring hospitalization. Five patients were treated for reasons other than symptoms: prior to planned procedure (3), positive culture in voiding patient (1), and a patient with a culture positive for Pseudomonas aeruginosa (1). Of patients with UTIs, 33.3% (4/12) had a negative urine culture at the time of UDS.
CONCLUSIONS: UTI after UDS is uncommon, with only a 1.5% incidence in this patient cohort. This calls into question the utility of routine urine culture. Clinical UTI within 30 days prior to UDS was predictive of need for treatment/UTI in this retrospective cohort. We have now developed a standard protocol/treatment algorithm with a standardized templated note that includes extractable data elements in the electronic medical record allowing for prospective data collection. This data will be used to refine our protocol, with the hope of targeting urine cultures to a high-risk subset of patients. 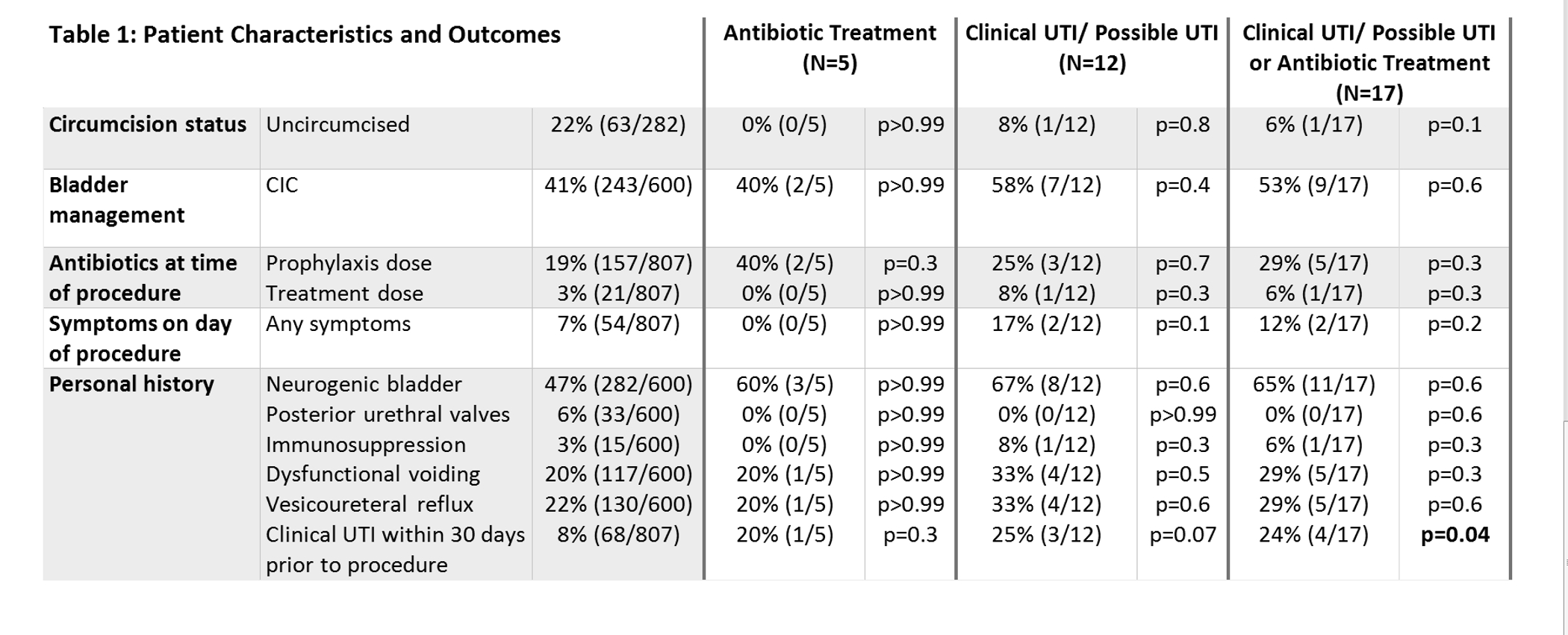
Back to 2016 Fall Congress
