Vesicoureteral Reflux Index (VURx): Predicting Primary Vesicoureteral Reflux Resolution in Children Diagnosed After Two Years of Age
Michael L. Garcia-Roig, MD1, Derrick E. Ridley, BS1, Courtney E. McCracken, PhD2, Angela M. Arlen, MD3, Christopher S. Cooper, MD3, Andrew J. Kirsch, MD1.
1Emory University/Childrens Healthcare of Atlanta, Atlanta, GA, USA, 2Emory University Department of Pediatrics, Atlanta, GA, USA, 3University of Iowa, Iowa City, IA, USA.
BACKGROUND:
The VURx, a 6-point weighted scoring system based on gender, timing of VUR on voiding cystourethrogram (VCUG), ureteral abnormalities, and VUR grade, is a validated scoring system designed to predict spontaneous reflux resolution or at least 2 grade improvement based on the initial VCUG in children diagnosed before two years of age. We aimed to assess whether the VURx predicts VUR resolution/improvement in children diagnosed after 2 years of age.
.
METHODS:
Electronic medical records from two institutions were queried for patients with primary VUR diagnosed at >24 months of age, with at least one additional VCUG prior to 18 years of age. Exclusion criteria included secondary VUR and interval between first and last VCUG >2 standard deviations from the mean of the cohort. The VURx scoring is: female - 1 pont; VUR timing: early/mid -3, late- 2; voiding only- 1; ureteral abnormalities(diverticulum, complete duplication)- 1; high grade VUR(IV/V)- 1. Resolution was defined as no VUR and improvement was ≥2 grade decrease in maximum VUR grade. Parametric survival models using the HAZARD procedure in SAS (v 9.3, Cary, NC) were used to identify variables associated with resolution/ improvement in the early (24 months) and later periods (>24 months) following diagnosis.
RESULTS:
271 patients (21M, 250F) met inclusion criteria with mean age at diagnosis of 4.0 ± 2.1 years and median VUR grade of 2. VUR timing was early/mid filling in 92(34.0%), late filling in 145(53.5%), and voiding only in 34(12.6%). Resolution/improvement by VURx score: 1- 1(100%); 2- 25(67.6%); 3- 48(37%); 4-18(21.4%); 5/6- 4(18.2%). Female gender (HR 0.22[95% CI 0.1-0.5], p< 0.001) and timing of VUR (late: HR 0.19[0.07-0.57], p=0.003; early/mid: 0.40[0.18-0.87], p=0.022) were significant predictors of non-resolution. Time to resolution (months) based on the VURx score was: ≤2: 15.6 months (95%CI 11.0-13.8); 3: 34.7 (25.4-44.1); 4; 55.9 (40.1-inf); ≥5: 30.3 (29.5-inf). High grade (IV/V) VUR was not predictive of resolution/improvement in early [HR 0.53(0.07-4.10)] or late [HR 0.94 (0.27 - 3.31)] periods. Ureteral abnormalities were associated with persistent VUR as no patient with them had early resolution/improvement (HR=0), and this was not associated with later resolution [HR 0.91 (0.30-2.75)]. BBD at diagnosis was not a significant predictor of resolution/improvement in both early [HR 0.94 (0.38-2.33)] and later [HR 0.71 (0.35-1.42)] time periods. A VURx score of 3 (HR 0.28[0.13-0.59], p=0.001) and 4 (HR 0.19[0.08-0.49], p< 0.001) predicted lack of resolution/improvement in early resolvers; however, the VURx and its components were not predictive of resolution/improvement in late resolvers (p>0.05). A parametric survival model of resolution/improvement by VURx score is illustrated in the Figure.
.
CONCLUSIONS:
VURx reliably predicts primary VUR resolution or >2 grade improvement in children diagnosed at ≥2 years of age. VUR resolution/improvement is significantly less likely to occur 24 months after diagnosis in these children. Further study is warranted to identify additional predictive components for the VURx in this population.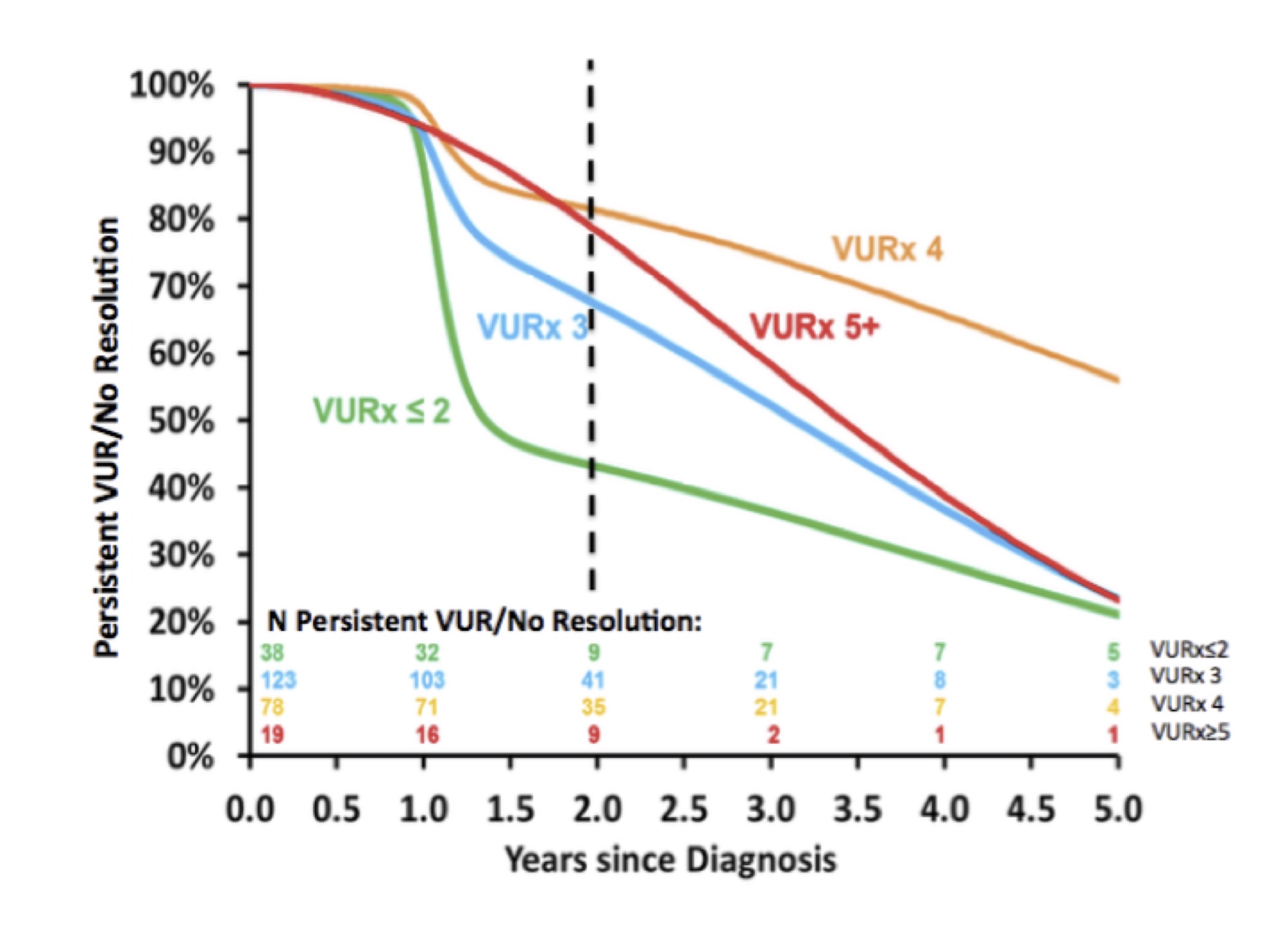
Back to 2016 Fall Congress
