Ultrasound Shear Wave Elastography: A Simple, Non-invasive Method to Evaluate Bladder Compliance
Renea M. Sturm, MD, Elizabeth B. Yerkes, MD, Jennifer L. Nicholas, MD, Devon Snow-Lisy, MD, Dawn Diaz Saldano, NP, P. Lacy Gandor, RDMS, Christopher G. Halline, BA, Ilina Rosoklija, MPH, Karen Rychlik, MS, Emilie K. Johnson, MD, MPH, Earl Y. Cheng, MD.
Lurie Children's Hospital, Chicago, IL, USA.
Introduction: Children with neurogenic bladder have an increased risk of upper urinary tract damage when intravesical storage pressures are elevated. The current evaluation of bladder compliance is invasive requiring catheterization and radiation exposure when videourodynamics is completed. Ultrasound shear wave elastography (SWE) is a non-invasive method to image the mechanical properties of soft tissue. It has previously been successfully applied to other organs to determine the presence and extent of tissue fibrosis. In this initial study, we sought to evaluate the use of SWE for a bladder application.
Methods: Children scheduled for routine urodynamics for neuropathic bladder were evaluated with concurrent SWE. Shear wave velocity (SWV) measurements were taken from the anterior (superior to pubic symphysis) and posterior bladder wall (midline trigone) when empty, at 25, 50, 75, 100% estimated bladder capacity (EBC) and end fill volume in the absence of detrusor contraction. Three regions of interest (ROIs) corresponding to each layer of the bladder wall were verified by a pediatric radiologist. One pediatric urologist assessed all urodynamic studies. Paired t-tests evaluated SWV from each site when the bladder was empty versus end fill volume. Pearson correlation coefficient and a mixed effects model (random effect for multiple observations per child, interaction term for mean SWV and %EBC) evaluated the relationship between SWV and intravesical pressure.
Results: Eighteen children (median age 12.5 years, range 5-23) were evaluated. Median end fill pressure or detrusor leak point pressure (EFP, DLPP) was 22cm/H20 (3-48). Utilizing National Spina Bifida Patient Registry (NSBPR) criteria, five bladders were categorized as normal or safe (EFP, DLPP<25cm/H20) and 13 intermediate or hostile (EFP or DLPP ≥25, NDO, DSD). In the 13 intermediate or hostile bladders, a significant increase in mean SWV of the anterior bladder wall occurred with filling (empty 1.49m/s ±0.11 standard error (SEM) vs end fill volume 2.01±0.12, p=0.007). However, there was no change in mean SWV from the anterior wall during filling in normal or safe bladders (1.46±0.05 vs 1.49±0.09, p=0.79). No significant change in mean posterior wall SWV with bladder filling occurred in either cohort. Figure 1 illustrates mean SWV from the anterior wall obtained at each endpoint in the two cohorts (figure 1: SWV vs EBC, error bars represent SEM at each endpoint, Capacity represents final measurements in bladders filled to 100 or 125%EBC).
In all 18 children evaluated, a significant relationship was observed between intravesical pressure and mean anterior SWV during filling (all endpoints ≥25%EBC, Pearson coefficient 0.69, p<0.0001). This relationship remained significant in the mixed effects model (p<0.0001).
Conclusions: SWV of the anterior bladder wall was significantly correlated with intravesical pressure in both compliant and noncompliant bladders. SWV increased with filling in intermediate/hostile as compared to safe/normal bladders. SWE is promising as a bedside modality that obviates the need for catheter placement or radiation exposure in the assessment of bladder wall changes associated with elevated intravesical storage pressures. 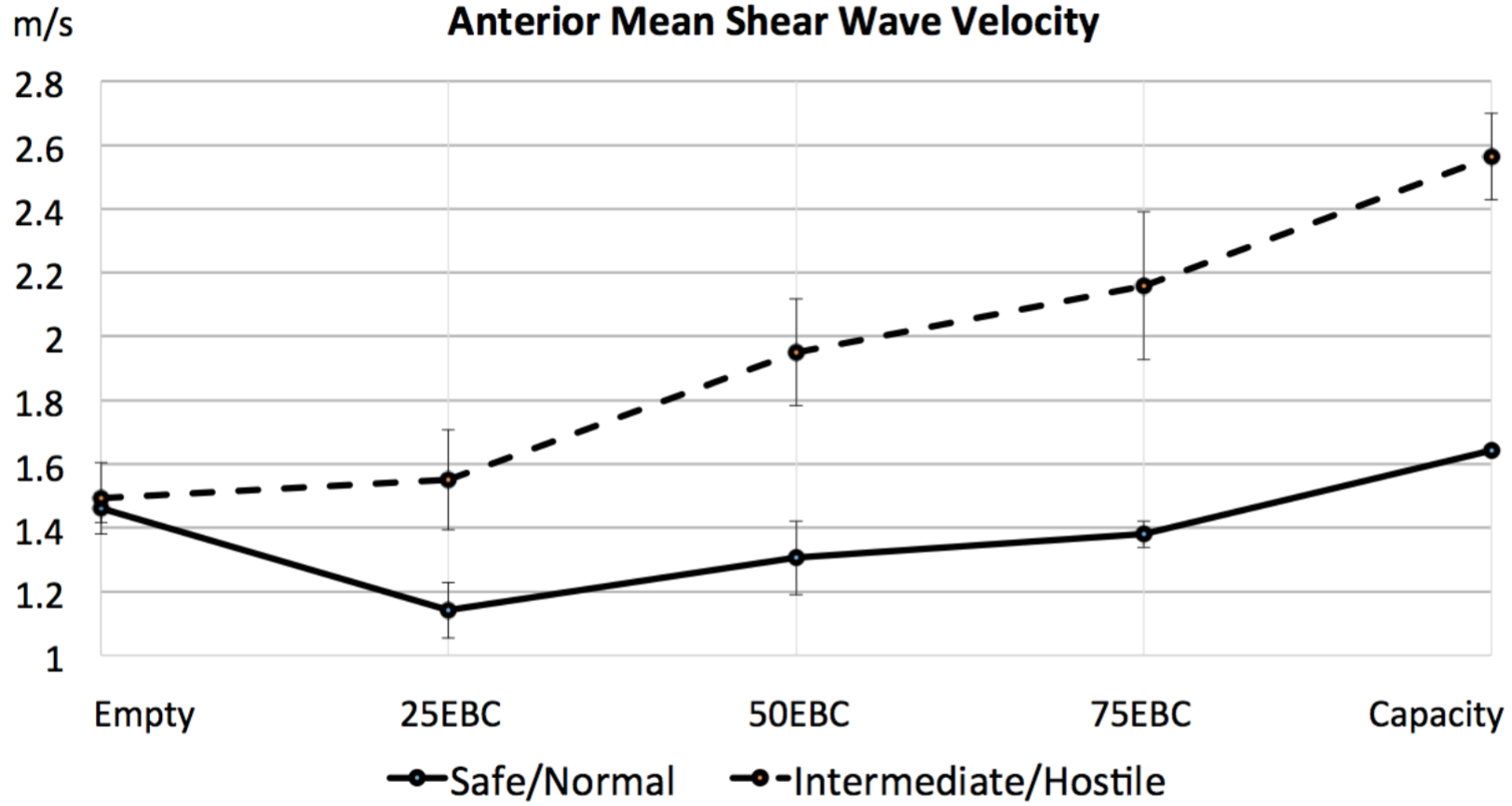
Back to 2016 Fall Congress
