Disparities in Access to Newborn Circumcision
Derrick Johnston, MD, Cynthia Sharadin, MD, Aaron Dahmen, MD, Joshua Earl, MD, Rhys Irvine, MD, Dana Giel, MD.
University of Tennesse, Memphis, OH, USA.
INTRODUCTION: Policy statements from the American Urologic Association and the American Academy of Pediatrics (AAP) confirm the medical benefits of newborn circumcision (NBC) and recommend presenting NBC as an option to families. The AAP policy statement further recommends insurance coverage for NBC which is not yet universal. Many boys who do not undergo NBC eventually undergo elective operative circumcision (OC). OC is more costly and carries increased risk due to need for general anesthesia. We hypothesize that socio-economic factors, including race and insurance status, influence access to NBC and OC.
METHODS: After IRB approval, records of newborn males (NBM) at our women’s hospital from 1/2000-6/2015 were evaluated. Demographics collected included ZIP code, language, race and insurance. If NBC was desired (indicated by signed consent in the records) but not performed, genital examination details were recorded along with reason for not performing NBC. A separate cohort undergoing OC in the same time period at our children’s hospital was identified. Intake forms of those requesting OC were reviewed to document why NBC was not performed. Pearson’s Chi-squared test was used for categorical variables. A binary logistic regression model was developed to evaluate continuous and categorical variables together.
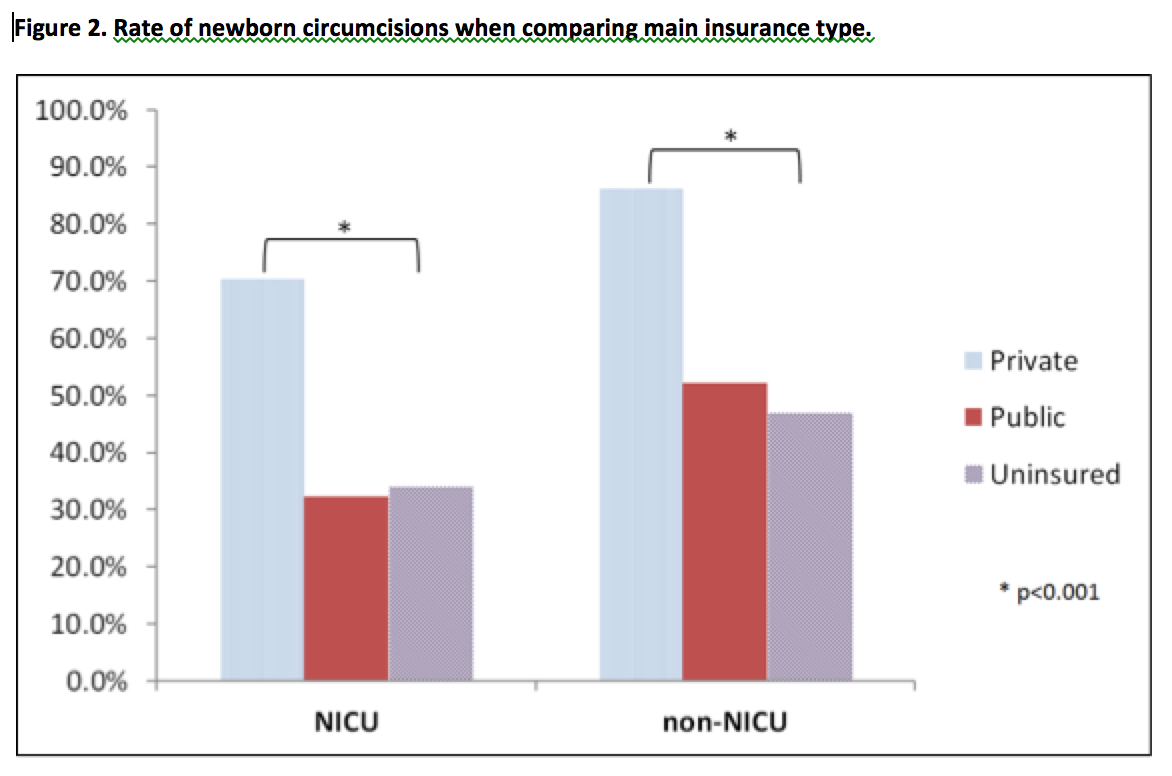
RESULTS: 14,960 NBM were identified. 10,776 (73.3%) underwent NBC. 67% had private insurance, 29.7% public insurance, and 3.2% were uninsured. The strongest predictor of NBC was private insurance with an odds ratio of 5.754 (P<.001). The difference in the rate of NBC between uninsured and publicly insured patients did not reach statistical significance (P=0.09). There was also an association between NCB and race. Whites were more likely to undergo NBC (p<.001) than other races. While admission to the NICU decreased the overall rate of NBC, the influence of insurance status and race remained with statistically significant differences persisting in this subgroup.
1,324 boys underwent OC during the same time period. 50% had private insurance, 49% public, and <1% were uninsured. 437 (33%) explicitly reported having sought NBC at birth. 129 (30%) of these patients reported no identifiable medical reason for not having NBC before discharge. Of those desiring but not receiving NBC, 88% had public insurance. This represents a shifting of care from NBC to OC which selectively impacts patients with public insurance.
CONCLUSIONS: NBC is a procedure with known benefit to which patients have unequal access. Insurance status and race have correlation with rates of NBC, supporting the hypothesis that these socioeconomic factors affect access to NBC. Patients who have been denied NBC often seek OC with its increased risk and burden of cost to the healthcare system. Access to newborn circumcision services represents a disparity of care in our healthcare system.

Back to 2016 Fall Congress
