The Effect of Sub-Specialization on Pediatric Surgical Complication Rates
Brian J. Young, MD, Rohit Tejwani, MS, Ruiyang Jiang, MD, Hsin-Hsiao S. Wang, MD, MPH, Steven Wolf, MS, Nathaniel H. Greene, MD, John S. Wiener, MD, J. Todd Purves, MD, PhD, Jonathan C. Routh, MD, MPH.
Duke University Medical Center, Durham, NC, USA.
Introduction: Increased case volumes and training are associated with better outcomes in pediatric surgery. We recently found increased pediatric sub-specialization among urologists was associated with decreased risk of surgical complications. We hypothesize that a similar association exists within other surgical specialties.
Materials & Methods: We analyzed the National Inpatient Sample from 1998-2009 to identify inpatient surgeries and National Surgical Quality Improvement Program (NSQIP) complications. We selected surgeons performing at least 50 cases per year and categorized them based on Pediatric Proportion Index (PPI): the ratio of pediatric (75%. We categorized pediatric surgical encounters based on standard HCUP Clinical Classification Software. Specialties included general pediatric surgery, neurosurgery, cardiothoracic, urology, orthopedics, and ENT. Encounters with simultaneous procedures across different specialties were excluded. Multivariate analysis was performed adjusting for age, gender, Van Walraven comorbidity score, insurance type, ZIP code median household income, year, and hospital location, type, size, and region to test for an association between PPI and post-operative NSQIP complication.
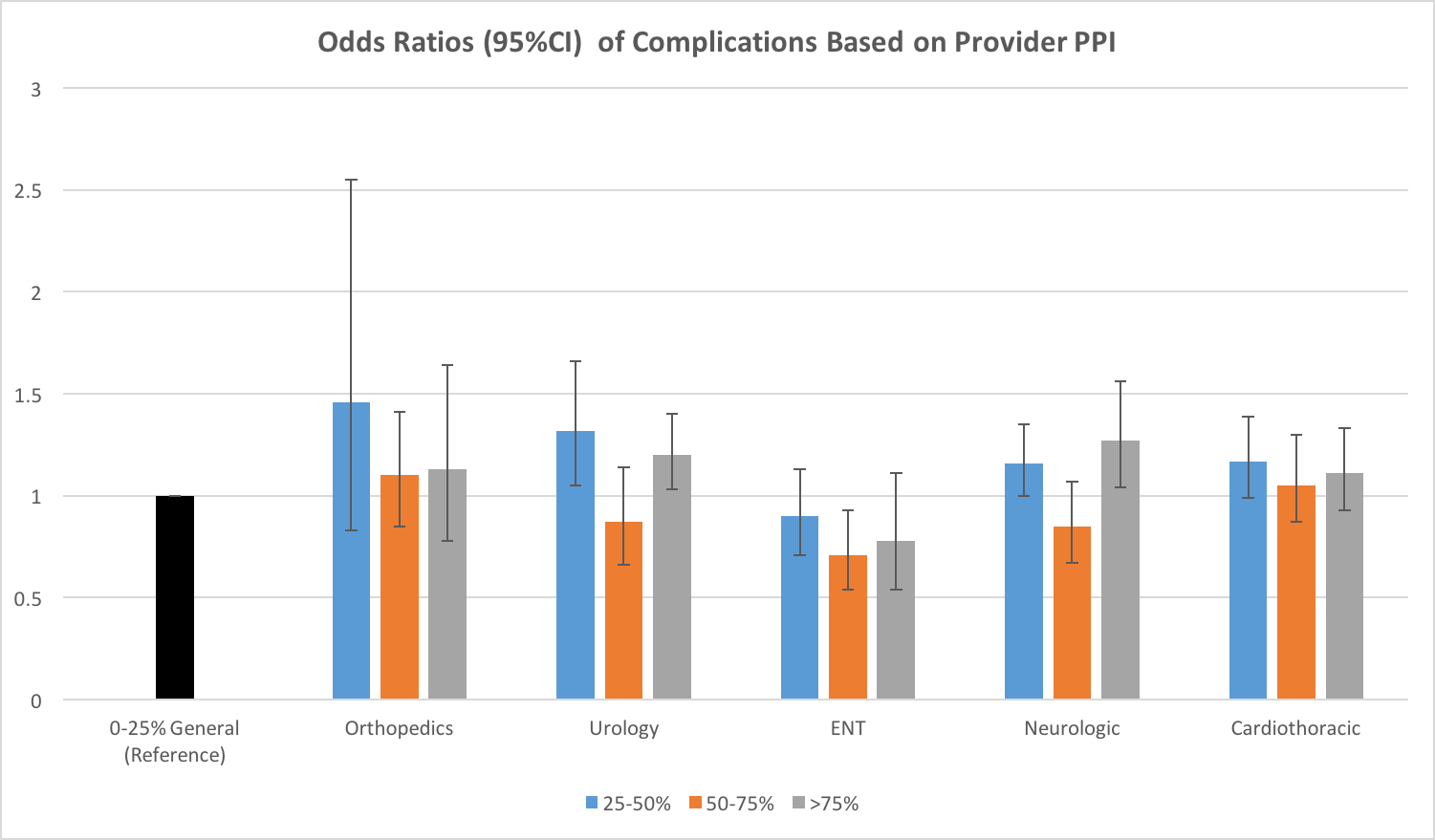
Results: We identified 2,269,461 weighted inpatient surgical encounters. 47% of inpatient pediatric surgeries were performed by surgeons with a PPI 75% (most specialized). Surgeons with the lowest PPI treated older children than those with the highest PPI (11.1 vs. 5.6 years, p75% compared to <25% (OR=0.86, CI: 0.77-0.96). Surgical sub-specialties had increased risk for complications relative to general pediatric surgery with the exception of orthopedics (p<0.001). Setting general surgeons with PPI<25% as a reference, all specialties trended toward lower complication risk as PPI increased (p<0.001). Across specialties we consistently found providers with a PPI of 50-75% to have the lowest odds of a post-operative complication (Figure).
Conclusions: Across various surgical specialties, providers whose practices are >50% dedicated to pediatrics have decreased complications when compared with surgeons who do relatively few pediatric procedures. We hypothesize that providers with a PPI of 50-75% have the lowest rate of complications due to their experience with routine cases coupled with the likelihood that the most complex cases are referred to the most specialized surgeons.. Further studies to validate this hypothesis using more clinically granular data sources are underway.
Back to 2016 Fall Congress
