Deciding Exit Strategy: A Short-Term Comparison of Externalized Pyeloureteral Stent Versus Internal Ureteral Stent in Pediatric Robotic-Assisted Laparoscopic Pyeloplasty
David Chu, MD, Dhirendra Shrivastava, MBBS, Jason Van Batavia, MD, Christopher Long, MD, Dana Weiss, MD, Aseem Shukla, MD, Arun Srinivasan, MD.
The Children's Hospital of Philadelphia, Philadelphia, PA, USA.
BACKGROUND: After pyeloplasty, urinary drainage options include traditional internal double-J (DJ) ureteral stents or externalized pyeloureteral (EPU) stents. A presumed benefit of the EPU stent is that it avoids an additional anesthetic exposure from DJ removal. We compared the short-term safety and efficacy of using a modified EPU stent, which is placed antegrade with the stent terminating mid-ureter, versus DJ stent on perioperative and postoperative outcomes following pediatric robotic-assisted laparoscopic dismembered pyeloplasty (RALP).
METHODS: We reviewed an IRB approved registry for children undergoing RALP and identified and analyzed consecutive cases performed beginning October 2013, when EPU stents began to be used, until September 2015. Data were collected on patient demographics, perioperative outcomes including operative duration and days hospitalized, and postoperative factors including complications, days stented, and flank pain following stent removal. Success was defined as stable or improved urinary tract dilation without flank pain on postoperative ultrasound obtained at least one month after stent removal. Bivariate statistical analyses were applied to compare the DJ versus EPU groups.
RESULTS: A total of 44 and 17 patients underwent DJ and EPU stenting, respectively, at the discretion of the operating surgeon. Median follow-up was 8.8 months (interquartile range [IQR] 4.2-13.5] from surgery. DJ patients were older than EPU patients (mean 8.5 vs 4.7 years, p=0.02), were less likely to be on postoperative antibiotic prophylaxis (23 vs 76%, p<0.001), and were more likely to experience gross hematuria postoperatively (25 vs 0%, p=0.03). EPU patients, compared to DJ patients, had no differences in postoperative success (100 vs 93%, p=0.55), operative duration (median 191 vs 198 min, p=0.62), or postoperative urinary tract infection (UTI) rate (6 vs 11%, p=1.00). All EPU stents were removed in the outpatient clinic setting without any complications. All DJ stents required an additional operation under anesthesia for removal.
CONCLUSIONS: Use of the EPU stent provides a safe alternative to DJ stenting and avoids the need for an additional anesthetic. The use of EPU stents also is associated with less gross hematuria while having comparable total operative time and short-term success. 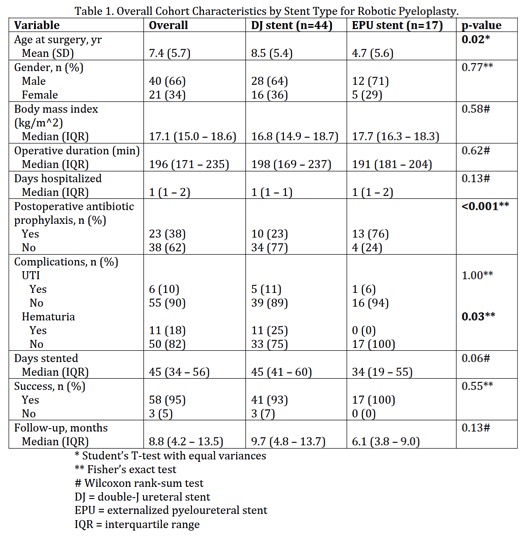
Back to 2016 Fall Congress
