Change in geometric measurement of pre-operative to post-operative renal ultrasound images predicts pyeloplasty success according to MAG3 scan: a blinded comparison to a gold standard.
Adam JM Kern, M.D., Bruce J. Schlomer, M.D., Micah A. Jacobs, M.D., M.P.H..
University of Texas Southwestern Medical Center, Dallas, TX, USA.
Background: After pyeloplasty for ureteropelvic junction (UPJ) obstruction, MAG3 diuretic renal scan remains the gold standard for determination of improvement in renal drainage. We hypothesized that the change in geometric measurements between preopearative and postoperative renal ultrasound images would predict pyeloplasty success.
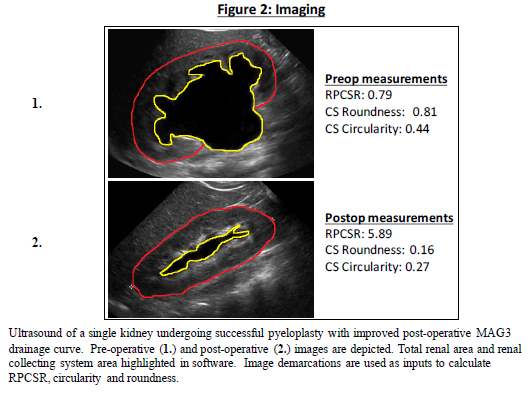
Methods: This study was an IRB-approved retrospective, blinded comparison to a gold standard. Included in the cohort were children age ≤18 years undergoing pyeloplasty at a single institution from 2009-2015, all having both pre- and post-operative MAG3 and renal ultrasound imaging. For each kidney, a representative preoperative and postoperative ultrasound image with longest cranial-to-caudal measurement that revealed renal pelvis was chosen. Our standard for pyeloplasty success was 1) improved drainage curve on MAG3 and, 2) lack of additional surgery. Measurements for collecting system circularity (4π(area/[perimeter2])), collecting system roundness (4×[(Area)/(π×(Major axis2))]), and renal parenchymal to collecting system area ratio (RPCSR) were obtained (Figure 1) on pre-operative and post-operative representative ultrasound images by 3 raters (Figure 2). Raters were blinded to timing of renal ultrasound and outcome of pyeloplasty. Changes in measurements between pre-operative and post-operative (roundness, circularity, RPCSR) were analyzed as a diagnostic test for pyeloplasty success using ROC curve analysis.
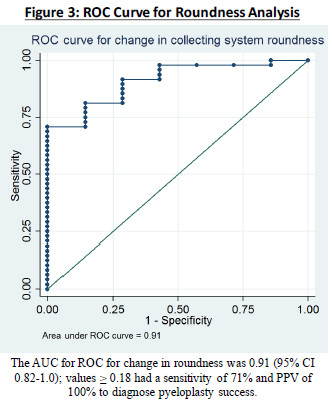
Results: 55 renal units that underwent pyeloplasty from 51 children were identified. There were 7 failures. Mean age at time of surgery was 4.9 years (range 0.2-17.6 years), with mean postoperative follow up time of 373 days. The AUC for ROC curve for change in RPCSR was 0.81 (95% CI 0.66-0.96); values ≥ 5.0 had a sensitivity of 50.0% and positive predictive value (PPV) of 100% to identify pyeloplasty success. The AUC for ROC for change in roundness was 0.91 (95% CI 0.82-1.0); values ≥ 0.18 had a sensitivity of 71% and PPV of 100% to identify pyeloplasty success (Figure 3). The AUC for ROC for change in circularity was 0.74 (95% CI 0.60-0.89); values ≥ 0.12 had a sensitivity of 45.8% and PPV of 100% to identify pyeloplasty success.
Conclusions: Pre-operative to post-operative change in geometric measurements of RPCSR, roundness, and circularity were able to predict pyeloplasty success, with change in roundness performing best. If the roundness score decreased at least 0.2 from preop to postop, this had 70% sensitivity and 100% PPV to identify pyeloplasty success. A decrease in collecting system roundness > 0.2 is highly predictive of improved MAG3 drainage after pyeloplasty and can be used to determine pyeloplasty success in lieu of MAG3 scan. 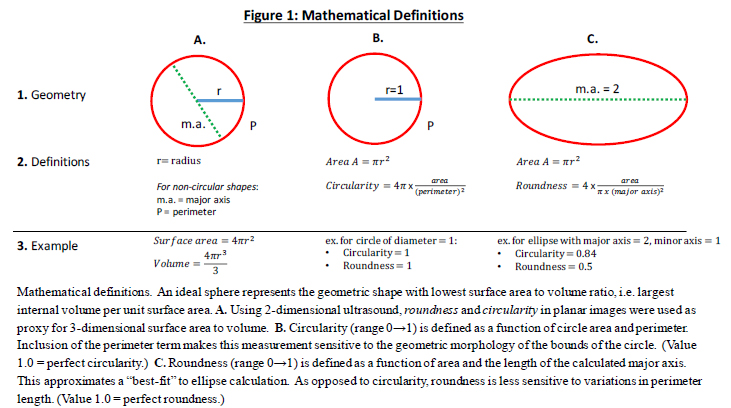
Back to 2016 Fall Congress
