Bladder Augmentation, Diversion and Clean Intermittent Catheterization in Classic Bladder Exstrophy: A 36-year Multi-Institutional Retrospective Cohort Study
Konrad M. Szymanski, MD, MPH1, Molly Fuchs, MD2, Daryl Mcleod, MD, MPH2, Ilina Rosoklija, MPH3, Andrew C. Strine, MD4, Brian VanderBrink, MD4, Benjamin Whittam, MD1, Elizabeth Yerkes, MD3, Patricio Gargollo, MD5, for the Pediatric Urology Midwest Alliance, (P.U.M.A.)6.
1Riley Hospital for Children at Indiana University Health, Indianapolis, IN, USA, 2Nationwide Children's Hospital, Columbus, OH, USA, 3Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, USA, 4Cincinnati Children's Hospital Medical Center, Cincinnati, OH, USA, 5The Mayo Clinic, Rochester, MN, USA, 6Pediatric Urology Midwest Alliance (P.U.M.A.), IL,IN, MN, OH, USA.
BACKGROUNDMuch bladder exstrophy literature consists of single-center series. Collaborative studies of rare conditions may offer insights by capturing practice heterogeneity and increasing statistical power. PUMA, a collaboration of 5 high-volume pediatric urology practices in the Midwestern United States, was created for this purpose. We aimed to assess (1) the risk of bladder augmentation and diversion (RAD) after primary bladder closure, and (2) prevalence of clean intermittent catheterizations (CIC) in a multi-institutional patient cohort.METHODS We conducted a retrospective cohort study of children born 1980-2016 with classic bladder exstrophy and managed in PUMA-affiliated centers. Those with less than 1 year of follow-up after birth, isolated epispadias, bladder exstrophy variants or anorectal malformations were excluded. The primary outcome was RAD after bladder closure. Subgroup analyses included: differences in RAD between institutions, birth cohorts (1980-1989, 1990-1999, 2000-2015) and RAD after primary bladder neck procedures (BNP). Secondary outcome was the proportion of patients performing CIC at last follow-up. Non-parametric tests and survival analysis were used. RESULTS Of 210 patients meeting inclusion criteria, 62.9% were male and 85.7% were Caucasian. Median follow-up was 13.9 years. Overall, 4 patients (1.9%) underwent primary diversion and 206 underwent primary closure (71.4% in first week of life). After primary closure, 104 (50.5%) underwent augmentation, 11 (5.3%) diversion and 91 (44.2%) had neither. Overall, 67.0% underwent a BNP, 26.1% of whom had a synchronous augmentation. On survival analysis, RAD was 14.9% by 5 years old, 52.0% by 10 years and 72.1% by 18 years. RAD varied significantly by center (p=0.047), but not by birth decade (p=0.31). RAD was 43.1% at 5 years after BNP. At last follow-up of the entire cohort, 65.7% of patients performed CIC. Among 91 with an intact native bladder, 28.6% performed CIC (73.1% via a channel). Probability of CIC did not differ between age groups (p=0.36). Among 104 augmented patients, 98.1% performed CIC (1.9% unknown), 87.1% via a channel. Older patients were more likely to use a channel (p=0.03). Among 71 adults without a diversion, 85.9% performed CIC (augmented: 100.0% CIC, native bladder: 28.6%). Fifteen patients were diverted (9 continent diversions, 4 ureterosigmoidostomies, 2 conduits). CONCLUSIONS We present long-term results of a large cohort of patients with classic bladder exstrophy. RAD increased with age: 1 in 2 patients by 10 years old and the majority by the time they reached adulthood. RAD differed between institutions. A fourth of patients, including adults, with a closed native bladder performed CIC. Looking at all adults, only 14% did not perform CIC.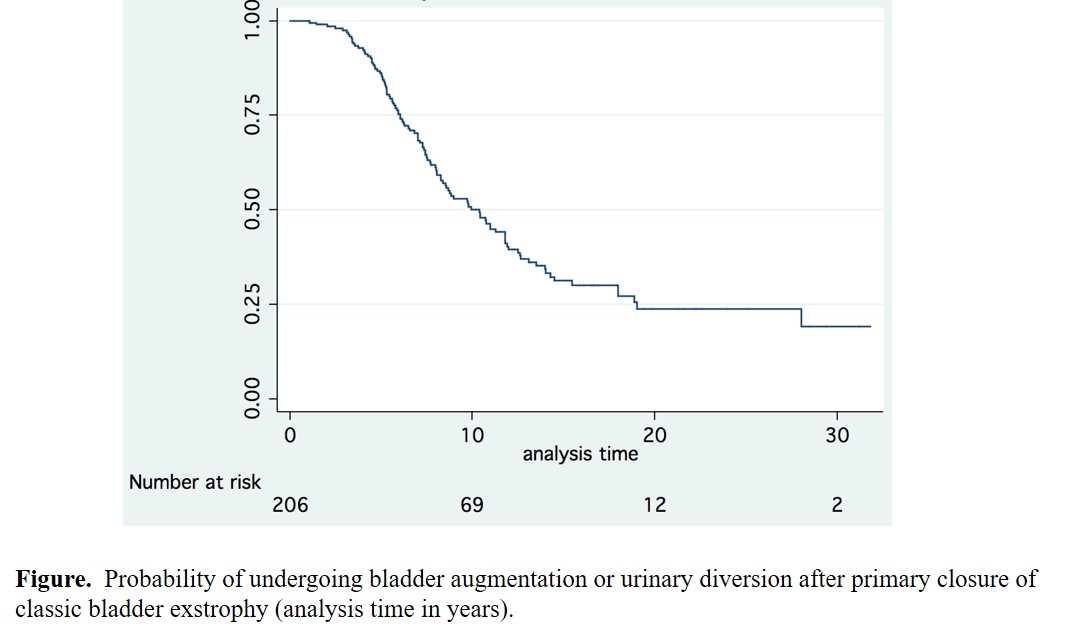
Back to 2017 Program
