Urology Referral and Progression to End-Stage Renal Disease: A Chronic Kidney Disease in Children (CKiD) Nested Case-Control Study
David I. Chu, MD1, Alison G. Abraham, PhD2, Christopher B. Pierce, MHS2, Michelle E. Ross, PhD3, Michelle R. Denburg, MD, MSCE1, Gregory E. Tasian, MD, MSc, MSCE1, Stephen A. Zderic, MD1, Susan L. Furth, MD, PhD1.
1Children's Hospital of Philadelphia, Philadelphia, PA, USA, 2Johns Hopkins Bloomburg School of Public Health, Baltimore, MD, USA, 3University of Pennsylvania Perelman School of Medicine, Philadelphia, PA, USA.
Introduction:
Children with chronic kidney disease (CKD) are at risk for progression to end-stage renal disease (ESRD). One modifiable factor for slowing CKD progression and improving outcomes is specialist care. Referral to nephrology has been associated with improved survival among patients with ESRD. Since the majority of CKD causes in children are related to congenital anomalies of the kidney and urinary tract, we explored the association of ESRD with referral to a pediatric urologist among children with CKD followed within the Chronic Kidney Disease in Children (CKiD) cohort. We hypothesized that patients who are referred to urology have less risk of ESRD.
Methods:
A nested case-control study was performed within the CKiD cohort, which is the largest prospective multi-center cohort of children ages 1-16 years with CKD in North America. Incidence density sampling matched cases of ESRD, defined as needing dialysis or transplant, to up to 3 controls on duration of time from CKD onset. Cases and controls were also matched on: sex, race, CKD etiology (glomerular versus non-glomerular), age at entry into CKiD, and history of low-birth-weight (<2500g). The primary exposure of interest was timing of urology referral: early (<1 year of age), late (>=1 year of age), or none. A secondary analysis examined the association between history of urologic procedure and ESRD. Sensitivity analyses examined only non-glomerular diagnoses. Conditional logistic regression analysis across matched sets was used to estimate rate ratios (RR) of the incidence of ESRD.
Results:
Of 130 cases within 704 total patients, 105 cases were successfully matched to 248 controls. Median age at CKiD entry was 13 years, 64% of diagnoses were non-glomerular in etiology, and median duration from CKD onset was 12 years. Univariable analysis showed that cases compared to controls had worse CKD stage and urine protein to creatinine ratio at CKiD entry and were less likely to have early urology referral or a prior urologic procedure (Table). Regression analyses demonstrated that no urologic referral compared to early referral was associated with a 2-fold increased risk of ESRD (RR 2.09 [95% Confidence Interval [CI] 1.04-4.17). No difference was seen between late or early referral (RR 1.04 [95% CI 0.48-2.23]). The increased risk of ESRD appeared driven by procedural intervention, with children denying any urologic procedure having greater than two-fold increased risk of ESRD compared to children who reported a prior urologic procedure (RR 2.23 [95% CI 1.23-4.05]). These findings were confirmed when restricted to non-glomerular diagnoses.
Conclusion:
Within CKiD, children with CKD who had no prior urology referral had significantly increased risk of ESRD compared to those who did see a urologist. The
reduction in risk associated with urology referral may be driven by procedural intervention particularly among children with non-glomerular causes of CKD.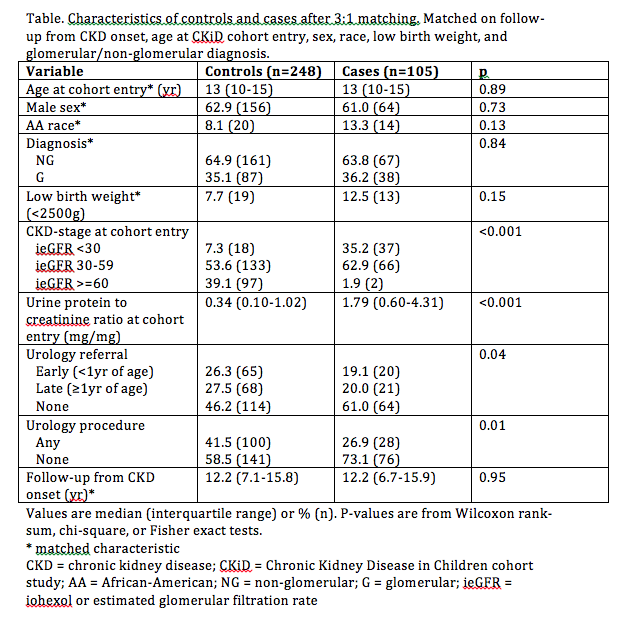
Back to 2017 Program
