Incidence And Risk Factors Associated With Venous Thromboembolism In Children Undergoing Surgery: A NSQIP-Pediatric Analysis
Jennifer Ahn, MD, Margarett Shnorhavorian, MD, MPH, Paul Merguerian, MD, MS.
Seattle Children's Hospital, Seattle, WA, USA.
BACKGROUND: Venous thromboembolic events (VTEs) are rare in the pediatric population, but its incidence is increasing. Known risk factors include malignancy, obesity, trauma, and immobility, but these studies focus on trauma and critical care patients. Post-surgical VTEs are well-studied in the adult population, and thus clear guidelines for prophylaxis and treatment exist. However, there are little data on post-surgical VTEs in the pediatric population. Our objective was to evaluate the rate of VTEs after pediatric surgeries and associated risk factors. We hypothesize that patients with baseline co-morbidities, longer anesthetic times, and immobility are at higher risk of developing post-operative VTE.
METHODS: The National Surgical Quality Improvement Program-Pediatric data from 2012-2015 were evaluated. Patients <18 years of age undergoing surgery were included, and the primary outcome was VTE requiring treatment (anti-coagulation or vena cava filter) within 30 days of surgery. Pre-operative patient characteristics, peri-operative details, and 30-day post-operative events were extracted. Characteristics of individuals with and without VTE were compared using t test and chi-square test. Univariate and multivariate logistic regression models were used to evaluate associations between VTE occurrence and explanatory variables. A p-value < 0.05 was considered significant. Analyses were performed using R. A subgroup analysis of Pediatric Urology patients was also performed.
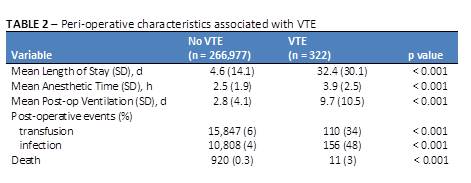
RESULTS: The overall incidence of VTE requiring treatment within 30 days of surgery was 12 per 10,000 individuals. For inpatient surgeries, the incidence of VTE was 20 per 10,000, while VTE occurred in 1.2 per 10,000 individuals undergoing outpatient procedures only. VTE was associated with female gender and several co-morbid conditions, including prematurity, malignancy, diabetes, developmental delay, cardiac disease, cerebral palsy, and bleeding disorders (Table 1). The incidence was higher in age categories of < 2 years and >10 years, consistent with the known bi-modal distribution of pediatric VTE. Regarding peri-operative characteristics, VTE was associated with longer anesthetic times, transfusions, post-operative infections, increased length of post-operative mechanical ventilation, and overall length of stay (Table 2). Median time to VTE event was 9 days (IQR: 5, 16). On multivariate logistic regression, malignancy, cerebral palsy, developmental delay, need for transfusion, and greater anesthetic time were associated with VTE events (p < 0.01).
For Pediatric Urology patients, the incidence of VTE was 2.6 per 10,000. VTE occurred after procedures including ureteral stent placement, appendico-vesicostomy, ureteroneocystostomy, and retroperitoneal lymph node dissection. Three of the patients (38%) had current malignancy, and anesthesia time was greater than two hours in 75% (6/8) of cases.
CONCLUSIONS: Post-operative VTEs in children and adolescents occur at rates similar to those of trauma patients, and are associated with similar risk factors. Identifying those at highest risk is crucial in creating guidelines for post-operative VTE prevention and treatment.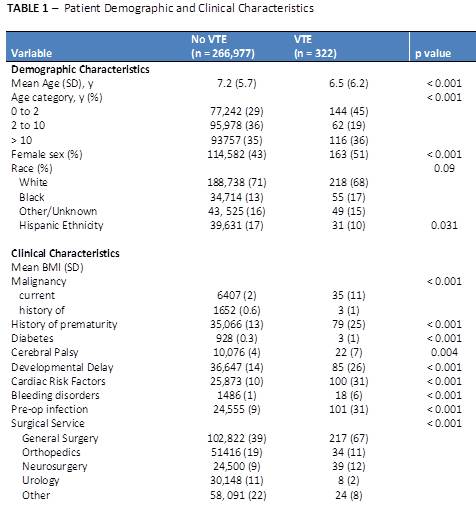
Back to 2017 Program
