Outcomes After Awake Spinal Anesthesia Vs. General Anesthesia With Caudal Block For Urologic Surgery In Infants
Emmett E. Whitaker, MD, Christopher J. Suozzi, BS, Seth A. Alpert, MD, Christina B. Ching, MD, Daniel G. DaJusta, MD, Daryl J. McLeod, MD, Venkata R. Jayanthi, MD.
Nationwide Children's Hospital, Columbus, OH, USA.
Introduction: Concerns regarding the potential neurotoxicity of general anesthesia (GA) in infants in addition to risks associated with airway management and postoperative apnea have prompted increased interest in alternatives to GA. This study reports outcomes at our institution after spinal anesthesia (SA) vs. GA + caudal block for urologic surgery in infants.
Methods: We performed a retrospective single, center analysis on patients who underwent SA or GA + caudal for urologic surgery (inguinal hernia repair, orchidopexy, orchiectomy) since September 2015. Patients were identified from our institution's spinal anesthesia database. An age- and procedure-matched control cohort was identified from a list of patients who underwent the above procedures under GA + caudal block. Outcomes recorded included success rate of SA, need for endotracheal intubation or laryngeal mask airway placement, need for anesthetics or narcotics in the OR, anesthesia time, surgery time, post-anesthesia care unit (PACU) time, time to recovery (as measured by the post-anesthesia recovery score (PARS), pain scores (as measured by the face, legs, activity, cry, consolability, or FLACC score, need for supplemental oxygen in the PACU, and need for analgesics in the PACU.
Results: A total of 68 patients were identified; 34 in the SA group and 34 in the GA + caudal group. Results for the two groups are summarized in Table 1 and Figure 1 (data expressed as mean + standard deviation). There was no significant difference with respect to mean age between the two groups (P=0.9928). When compared with GA + caudal, SA was associated with significantly less anesthesia time (P=0.0001) and surgery time (P=0.0004), but not less PACU time (P=0.3356). In addition, SA was associated with lower average pain scores in PACU (P=0.0015) and more rapid recovery (P=0.0071). Only one patient in the SA group required airway intervention (nasal cannula), while every patient in the GA + caudal group required intubation or placement of a laryngeal mask airway. 9/34 (26%) of patients in the SA group received anesthetics and/or narcotics in the OR compared to 34/34 (100%) in the GA + caudal group. No patient in the SA group required analgesics in the PACU compared to 14/34 (41%) in the GA + caudal group. Finally, no patient in the SA group required airway intervention or supplemental oxygen compared to 29/34 (85%) in the GA + caudal group. Of these, 22/29 (76%) received blow-by oxygen therapy, 6/29 (21%) required temporary continuous positive airway pressure, and one patient required reintubation.
Conclusions: Our retrospective data suggest that SA is associated with several benefits when compared to a more typical anesthetic regimen for these urologic procedures. SA should be considered as a safe, efficacious, and potentially superior alternative to GA + caudal block.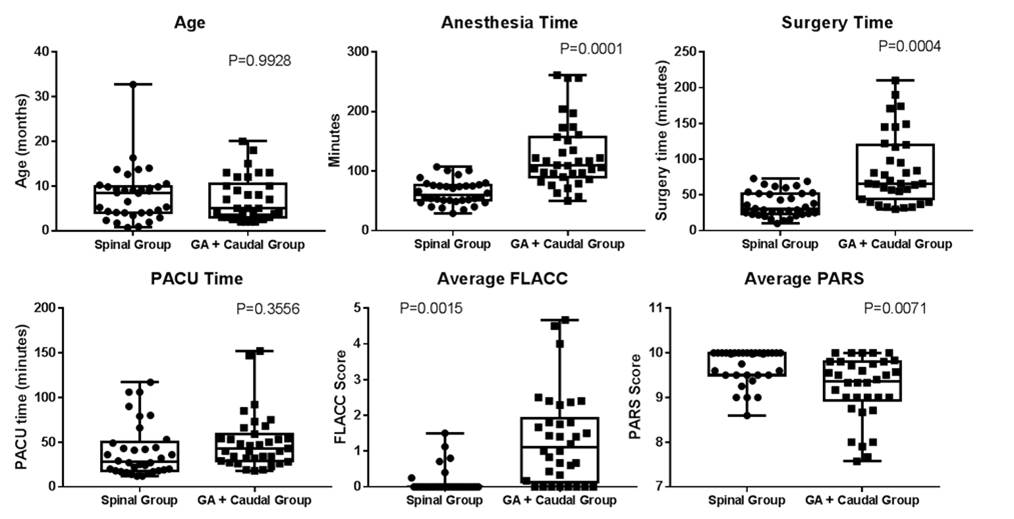
| Spinal Group | GA + Caudal Group | P-value | |
| Age (months) | 6.9 + 5.9 | 7.0 + 4.9 | 0.9928 |
| Anesthesia time (minutes) | 64.1 + 20.0 | 126.4 + 55.1 | 0.0001 |
| Surgery time (minutes) | 37.0 + 17.8 | 86.1 + 49.7 | 0.0004 |
| PACU time (minutes) | 40.4 + 29.8 | 50.6 + 31.0 | 0.3556 |
| Average PARS | 9.72 + 0.387 | 9.21 + 0.705 | 0.0071 |
| Average FLACC | 0.14 + 0.35 | 1.32 + 1.28 | 0.0015 |
Back to 2017 Program
