Durability of Pediatric Robotic Pyeloplasty: Are Long Term Clinical and Imaging Follow Up Protocols Necessary?
Courtney K. Rowe, MD, Michael E. Shapiro, BS, Jonathan S. Ellison, MD, Thomas S. Lendvay, MD.
Seattle Children's Hospital, Seattle, WA, USA.
BACKGROUND: Robot-assisted laparoscopic pyeloplasty is an established treatment for ureteropelvic junction (UPJ) obstruction. However, the literature in children is limited to short-term follow-up and the benefit of long-term imaging in post-operative patients is unclear. We report our long-term outcomes after robotic pyeloplasty over a 10-year experience. We hypothesized that continued follow up would uncover continued surgical failures.
METHODS: We utilized IRB-approved retrospective and prospective databases of patients who underwent robotic pyeloplasty at our institution since 2006. Inclusion criteria were any patient with available post-operative imaging. Success was defined as improvement in post-operative imaging, improvement in pain with stable imaging, or a non-obstructive post-operative MAG3 Lasix renogram. Failures were defined as patients who required a revision pyeloplasty on the affected UPJ due to concern for obstruction. Clinical length of follow-up was calculated to the most recent symptom check in clinic or by phone. Our long-term cohort was defined as any patient with more than 5 years clinical follow-up.
RESULTS: 169 patients underwent robotic pyeloplasty between 2006 and 2016. Of these, 146 met inclusion criteria and 36 had long-term follow (5.2 - 10.1 years). Most patients in the long-term cohort were boys (72%) and one patient (2.8%) had prior surgery on the UPJ. Median age at time of surgery was 83.5 months (4 - 215). One surgeon performed 94% of the operations using the dismembered pyeloplasty technique for most (80%). Median operative time for the long term cohort was 210 minutes (128 - 388) and median length of stay was 2 days (1 - 8) with 44% of patients discharged POD1. There was one intra-operative complication, a small bowel serosal tear. Most patients had an intra-operative stent (97%) with median stent duration 33 days (10 - 99). Within the long-term cohort, five (14%) patients experienced post-operative complications, some multiple. Overall, 92% of pyeloplasties were successful long term.
There were three patients who required a redo operation in the long-term cohort. All of these failures presented with flank pain including two who had been followed annually with reassuring ultrasound imaging. The longest interval between initial surgery and redo operation was 7 years. The long-term failure rate was similar between the long-term cohort and the overall cohort which had a total of six failures, only one presenting asymptomatically with worsening hydronephrosis on immediate post-operative imaging (Figure 1).
CONCLUSIONS: Robot-assisted laparoscopic pyeloplasty is safe and durable in pediatric patients but since failures can present years after the initial surgery, continued follow up is important. With only one patient in the full cohort presenting with asymptomatic failure, it remains to be seen whether long-term imaging is required or clinical follow up alone will suffice. Further study and multi-institutional collaborations will be required to truly understand the comparative effectiveness of robotic pyeloplasty.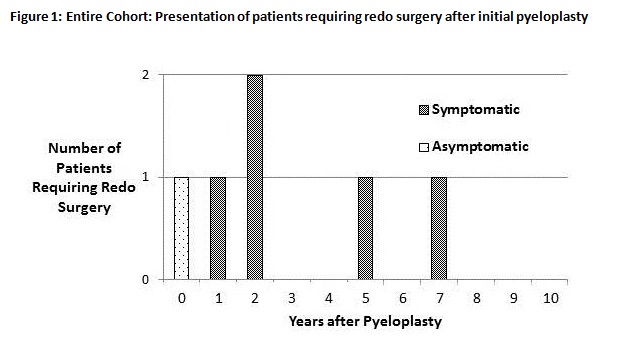
Back to 2017 Program
