Scar Acceptance After Pediatric Urologic Surgery
Mary K. Wang, MD, Yi Li, MD, Laurence Baskin, MD.
University of California San Francisco, San Francisco, CA, USA.
Introduction: We aim to survey patients to evaluate their personal opinions regarding their scar size, shape, and degree of bother, as these scars are known to grow over time. The purpose of the study is to evaluate the evolution of surgical scars from the neonatal period and early childhood through the teenage years in order to help guide parents and surgeons in making the best surgical approach decisions for neonatal patients.
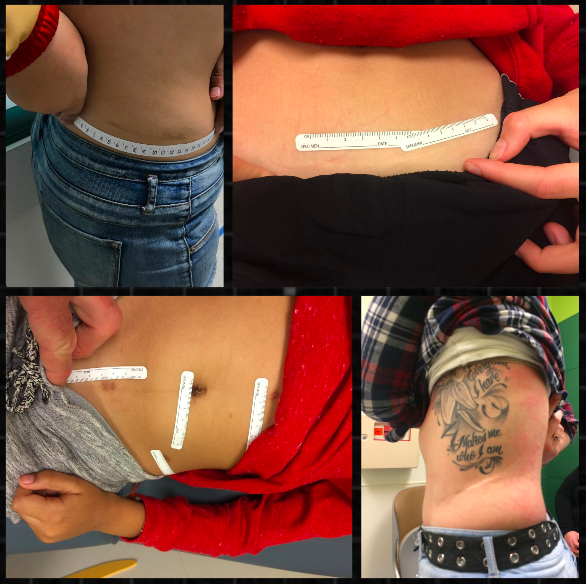
Materials and Methods: This was a cross-sectional study where patients who have undergone urologic surgery by a single surgeon at a young age are evaluated years later for scar satisfaction. Pictures of scar length using rulers and photography were employed as part of the study design. An abbreviated validated questionnaire was given to both parents and patients regarding their interpretation of scar length, satisfaction or bother. Percent change of scar length was calculated via normalized abdominal circumferences that were age and gender matched to assess for growth status over time.
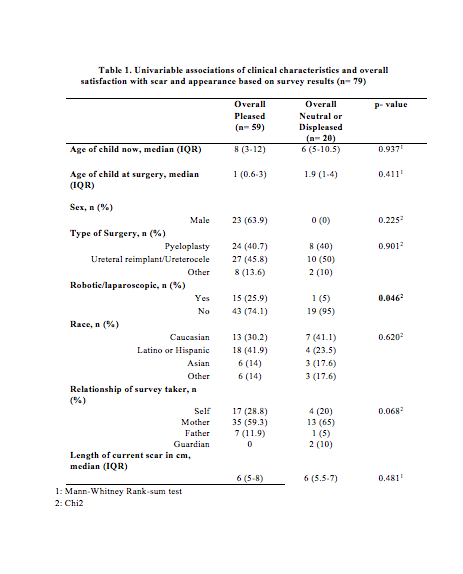
Results: 98 surveys were obtained regarding 74 children who underwent pediatric urologic surgery. Median age at the time of surgery and at the time of the study was 1.2 years and 7.5 years, respectively. Pyeloplasty (47.3%) was the most commonly performed surgery followed by ureteral reimplantation/ureterocele (43.2%) and other (9.5%). Patients and parents interpreted current scar length as very short (30.4%), short (53.2%), long (16.4%), and very long (0%). Bother was a minimum with 83.5% of families reporting no bother and only one patient reporting moderate bother. Overall, only surgical approach (robotic/laparoscopic vs open) seemed to influence whether families reported very pleased/pleased versus neutral/somewhat bothered attitudes towards the scar outcome (p=0.046). The median scar length was 4.5cm at time of surgery and 6cm (IQR 5-8) currently. Median percent change of scar length was 0.9% (IQR 0.2-2.9) in relation to age matched abdominal circumference. Kruskal-Wallis analysis demonstrated that percent change of scar length varied compared to the type of open surgery was statistically significant (p=0.05) with flank incisions growing a median of 1.1% versus 1.9% for Pfannensteil incisions. By race, "other" experienced the highest percent change 2.3%, then Hispanic/Latino 1.4%, Caucasian 0.9% followed by Asian -0.25% (p=0.01).
Conclusions: The majority of families and patients are pleased with their overall scar appearance after undergoing major pediatric urologic surgery despite location or length of scar. Scars tend to grow in length overtime but percent change of total abdominal circumference was less in Caucasian and Asian children and those who underwent minimally invasive surgery or open flank incisions.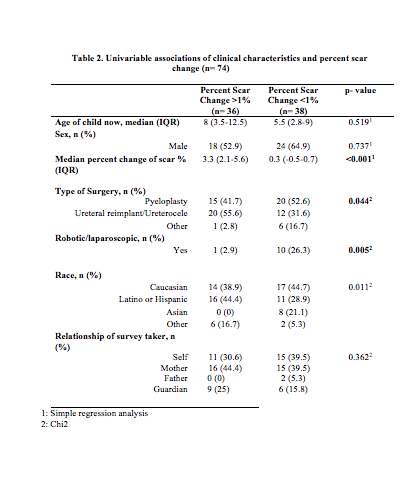
Back to 2017 Program
