-->
|
Back to 2014 Fall Congress Meeting Abstracts
How to decide which infant can have robotic surgery? Just do the math.
Julia B. Finkelstein, MD, Alison C. Levy, BA, Mark V. Silva, MD, Lauren Murray, CPNP, Christina Delaney, CPNP, Pasquale Casale, MD.
Columbia University, College of Physicians and Surgeons, New York, NY, USA.
Background: In pediatric urology, robotic assisted laparoscopic surgery has overcome several impediments of conventional laparoscopy. It has been previously reported that, in an artificial environment, collisions occurred more frequently in smaller workspace. There is currently no consensus on which infants can undergo robotic intervention, and furthermore no parameters to assist in decision-making. We evaluated our experience with infants to create an objective standard to determine which patients are most suitable for robotic surgery.
Methods: We prospectively evaluated 45 infants, aged 3 to 12 months of age, who underwent a robotic intervention for either upper or lower urinary tract pathology. At the preoperative office visit we measured the distance between both anterior superior iliac spines (ASIS) as well as the puboxyphoid distance (PXD). We then recorded the number of robotic collisions as well as console time. All surgeries were performed utilizing the da Vinci Si Surgical System by a single surgeon.
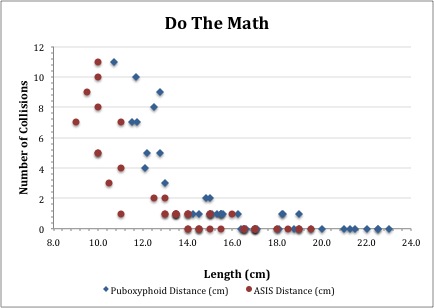
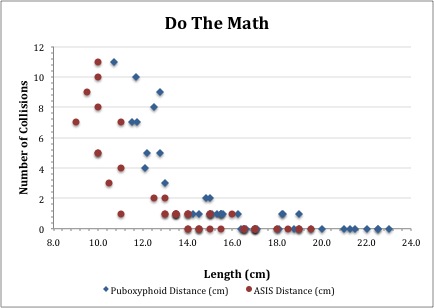
Results: There were 24 males and 21 females. There were no differences in ASIS, PXD, collisions or console time stratified by gender. Mean age was 6.6±1.6 months. There was no significant correlation between age and number of collisions (r = -0.242, p = 0.11). Similarly, there was no correlation between age and console time (r = -0.184, p = 0.23). Mean console time was 87.5±31.4 min. The median number of collisions was 1 (range 0-11, mean 1.9±3.0). There was a strong inverse relationship between ASIS distance and the number of collisions (r =-0.775, p < 0.001). There was also a strong inverse relationship between PXD and collisions (r = -0.746, p < 0.001). Additionally, there was a strong correlation between number of collisions and console time (r = 0.768, p < 0.001).
Dividing the cohort into few collisions (zero or one) versus several collisions (two or more), the ASIS and PXD were significantly smaller in those patients with several collisions (ASIS: 10.5 vs. 15.3 cm, p < 0.001; PXD: 12.6 vs. 17.9 cm, p < 0.001). Put another way, using a cutoff of 13.5 cm for the ASIS, there were significantly fewer collisions in the ≥ 13.5 cm group as compared to the < 13.5 cm group (0.4 vs. 5.1 collisions, p < 0.001). This was also true for the PXD using a cutoff of 15 cm: there were significantly fewer collisions in the > 15 cm group as compared to the ≤ 15 cm group (0.3 vs. 4.8 collisions, p < 0.001).
Conclusions: We found that surgeon ability to perform robotic surgery in an infant is restricted by collisions when the patient has an ASIS measurement of 13.5 cm or less or a PXD of 15 cm or less. Our objective assessment of puboxyphoid and ASIS distance is the best parameter to aid in selecting which infants can safely undergo robotic intervention with a minimum of instrument collision, thereby reducing operative time.
Back to 2014 Fall Congress Meeting Abstracts
|