-->
|
Back to 2014 Fall Congress Meeting Abstracts
Does channel type and stomal location affect long-term outcomes of catheterizable continent urinary channels?
Konrad M. Szymanski, MD, Benjamin Whittam, MD, Rosalia Misseri, MD, Chandra K. Flack, MD, Martin Kaefer, MD, Richard C. Rink, MD, Mark P. Cain, MD.
Riley Hospital for Children, Indianapolis, IN, USA.
BACKGROUND: Appendicovesicostomy (APV) and Monti ileovesicostomy (Monti) are commonly used catheterizable channels. Previous reports demonstrate similar rates of subfascial revisions between APV and Monti with short-term follow-up. The goal of this study was to assess durability of the APV and Monti in a large cohort with long-term follow-up.
METHODS: We performed an IRB-approved retrospective review of consecutive patients under 21 years old undergoing an APV and Monti surgery at our institution (1990-2013). We collected data on demographics, channel type, stomal location, channel continence along with stomal and subfascial revisions. Kaplan-Meier survival and Cox proportional hazards analysis were used.
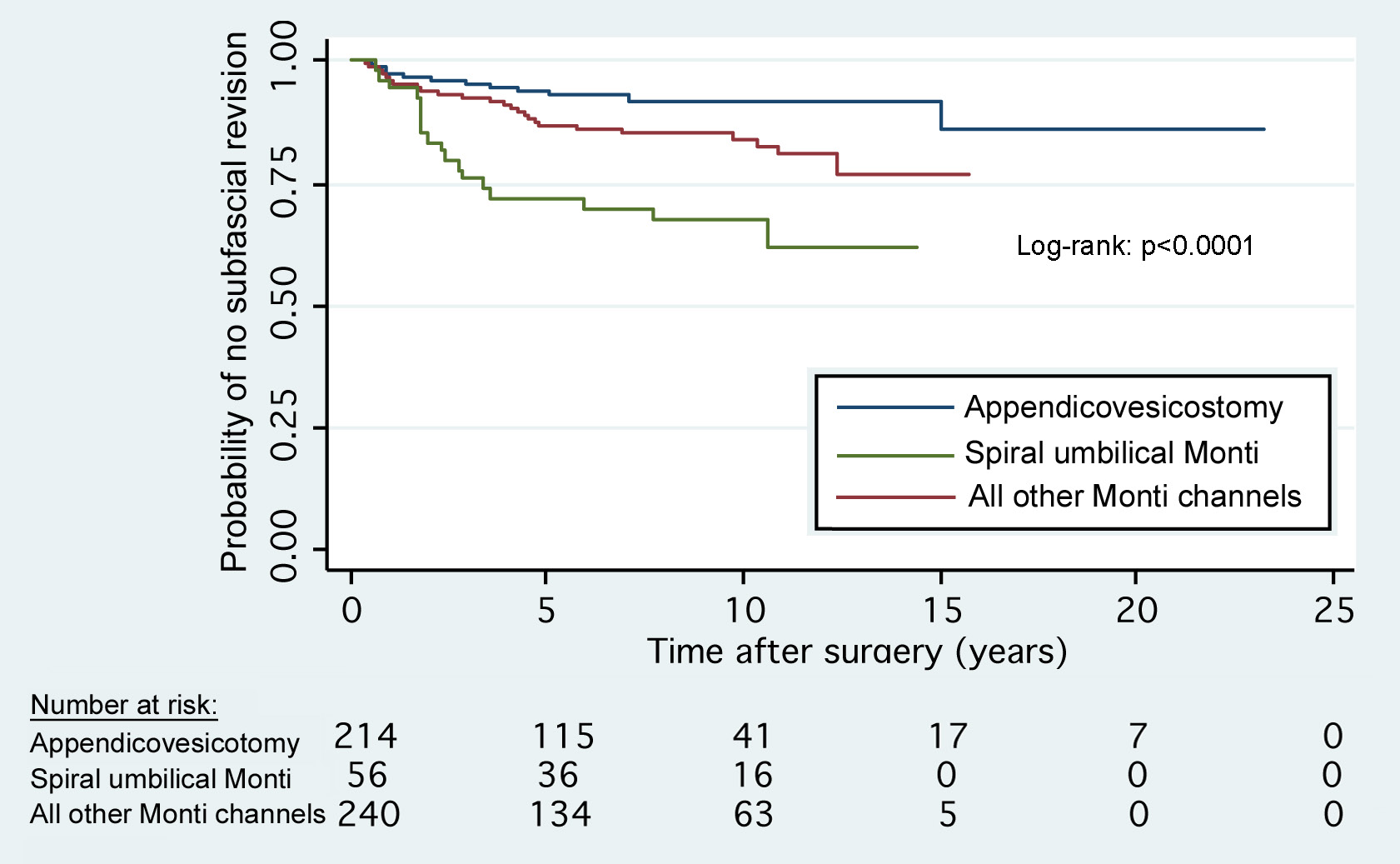
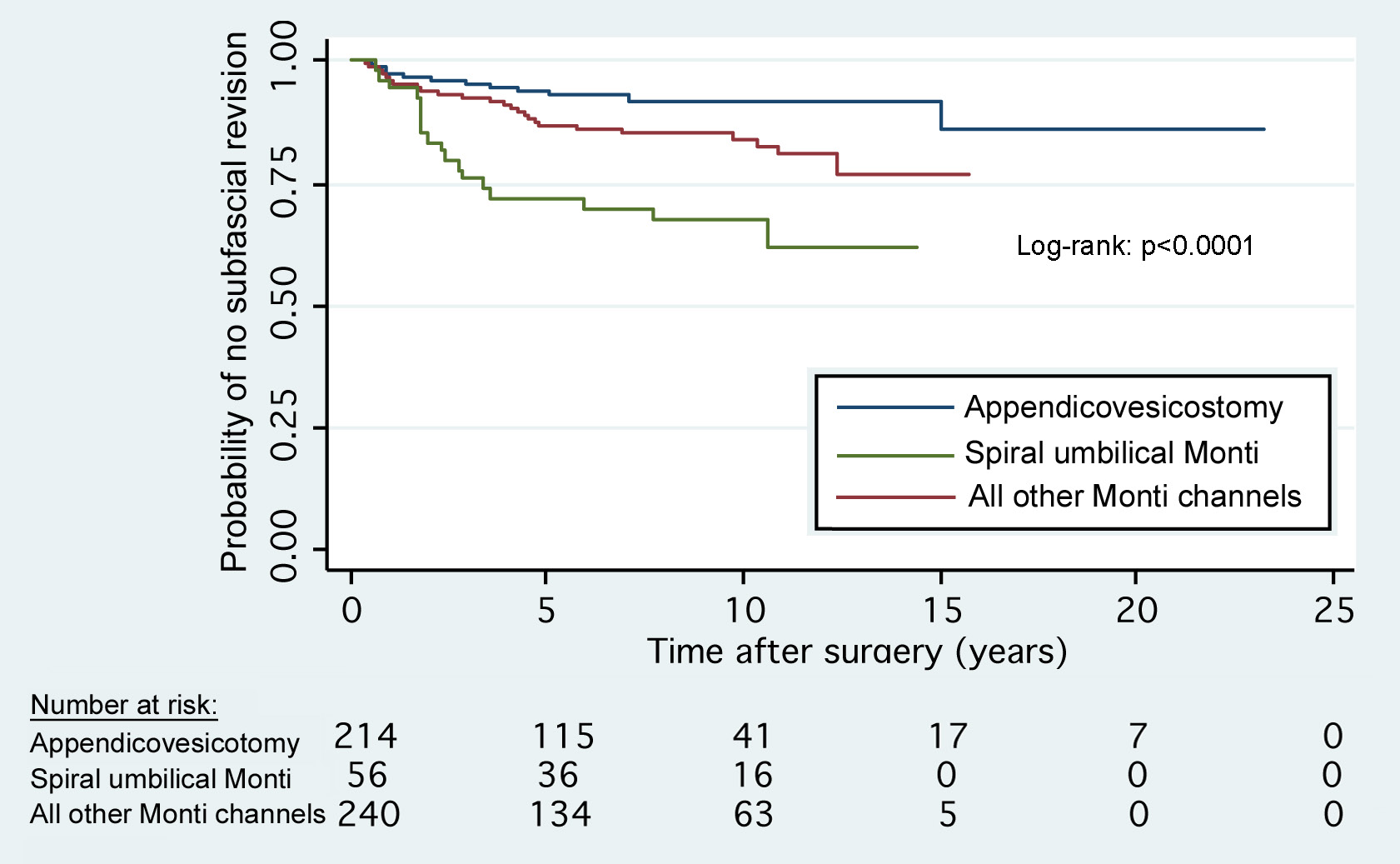
RESULTS: Of 510 patients meeting inclusion criteria, 214 patients had an APV and 296 had a Monti (50.5% spiral Monti). Median age at surgery was 7.4 years for APV and 8.7 years for Monti. Median follow up was 5.7 years for APV and 7.7 years for Monti. Stomal stenosis and channel continence for APV vs. Monti were similar (7.5% vs. 7.4%, p=0.99, 98.1% vs. 96.6%, p=0.41, respectively). Fourteen APVs (6.5%) had subfascial revision compared to 49 Montis (16.6%, p=0.001). On survival analysis, subfascial revision probability at 10 years for the APV was 8.6%, Monti channels excluding spiral umbilical Monti: 15.5% and spiral umbilical Monti: 32.3% (p<0.0001, Figure 1). On multivariate regression, Monti was 2.12 times more likely than APV to undergo revision overall (p=0.03). The spiral Monti to the umbilicus, in particular, was 4.66 times more likely than the APV to undergo revision (p=0.03). Gender, age at surgery, date of surgery and diagnosis of myelomeningocele were not significant predictors of subfascial revision, while stomal location was significant only for the spiral Monti (p≥0.17).
CONCLUSIONS: We demonstrate durable, long-term results with the APV and Monti techniques in a large cohort with long-term follow-up. The risk of channel complications continues over the channel’s lifetime and is more than twice as high in Monti than APV.
Back to 2014 Fall Congress Meeting Abstracts
|