-->
|
Back to 2014 Fall Congress Meeting Abstracts
Time to resolution of prenatal urinary tract dilation according to the severity of renal pelvis APD and SFU criteria: a prospective study
Luis H. Braga, MD, MSc, PhD1, David M. Kanters, BSc1, Forough Farrokhyar, PhD1, Julia Pemberton, MSc, PhD(c)1, Armando Lorenzo, MD2.
1McMaster University, Hamilton, ON, Canada, 2Hospital for Sick Children, Toronto, ON, Canada.
Background:
Both the SFU grading system and APD of the renal pelvis have been used to classify the severity of prenatally detected urinary tract dilation (UTD). Resolution trends, a commonly employed endpoint, are clearly time-dependent and expected information to be provided during counseling. Herein we examine how these systems discriminate and compare in predicting the natural progression of prenatal UTD, analyzing data from a prospective cohort.
Methods:
We screened 502 patients less than 24 months of age with prenatal UTD who were referred to a Pediatric Urology outpatient clinic between August 2009 and March 2014. Patients with duplication anomalies (119), posterior urethral valves (31), neurogenic bladders (17), Prune-Belly (1), and those who had surgery (56) were excluded. SFU grade and APD of the most severely dilated hydronephrotic kidney collected at baseline and at each visit were compared to identify trends in 278 consecutive eligible patients. UTD resolution was defined as SFU grade I or 0 or APD < 10mm. Resolution rates among SFU grades (I-IV) and APD ranges (10-15 versus greater than 15mm) were compared using Pearson Chi-square. Time to resolution was analyzed using Kaplan-Meier curves and log-rank tests.
Results:
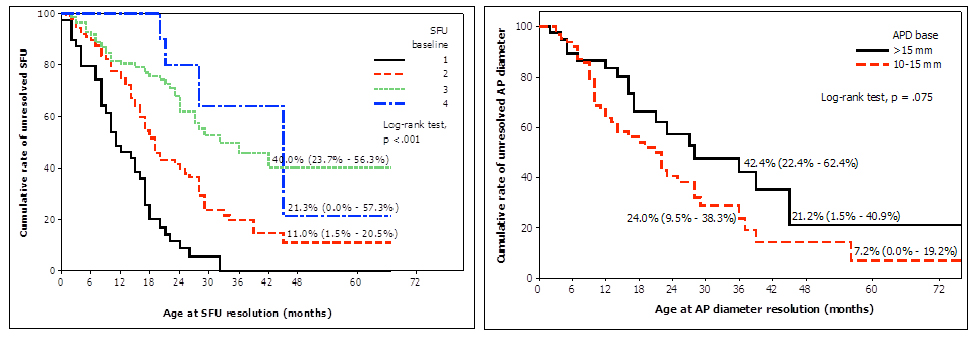
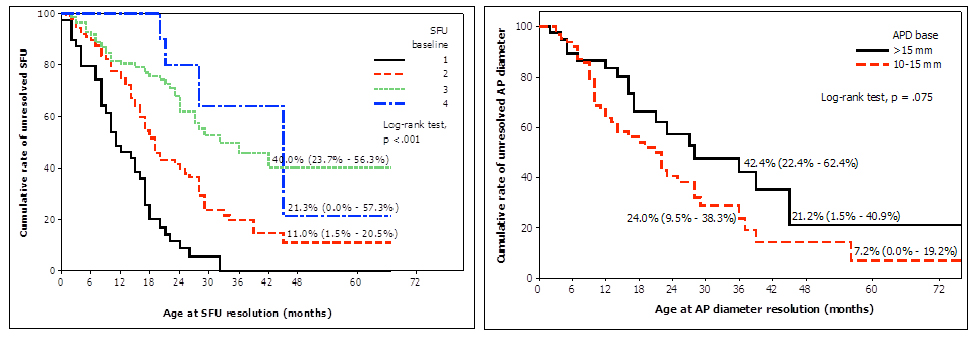
Mean age and mean APD at enrollment were 4.5±4 months and 10±5 mm, respectively. Of 278 (221, 80% male) children, 142 (51%) downgraded their UTD to SFU grade I or 0 and 207 (75%) reduced their APD to less than 10mm over a mean follow-up time of 16±10 months; 5/21 (24%) SFU grade IV patients resolved their UTD after a mean follow-up of 32±12 months, 39/121 (32%) SFU grade III resolved over 15±10 months, 60/98 (61%) SFU grade II resolved after 17±10 months, and 38/38 (100%) SFU grade I resolved over 12±8 months. 98/136 patients with SFU I/II improved vs 44/142 with SFU III/IV (72% vs 31%, p<0.01). Of 43 children with baseline APD greater than 15mm, 20 (47%) resolved their UTD after a mean follow-up of 21±14months, while 42/79 (53%) with 10-15mm APD improved over 16±11 months. 106/190 patients with isolated hydronephrosis (UPJO-like) resolved their UTD vs 12/45 with hydrouteronephrosis (primary megaureter) (56% vs 27%, p<0.01). Kaplan-Meier curves showed that patients with different baseline SFU grades had significantly different resolution times for their UTD (p<0.01) (Figure 1A). Differences in resolution rates were also observed for children with APD greater than 15mm vs those with 10-15mm APD, although not statistically significant (p<0.07) (Figure 1B).
Conclusions:
In a time to event analysis, SFU grading system was able to discriminate the likelihood of UTD resolution better than APD criteria. Our data presents information that is valuable during counseling, providing resolution rates which take into account duration of follow-up based on rigorously, prospectively collected information.
Back to 2014 Fall Congress Meeting Abstracts
|