-->
|
Back to 2014 Fall Congress Meeting Abstracts
Clinical Effectiveness of Orchidometry in Boys with Varicocele
Michael P. Kurtz, MD, MPH, Matthew Migliozzi, MA, Ilina Rosoklija, MPH, David Zurakowski, PhD, David A. Diamond, MD.
Boston Children's Hospital, Boston, MA, USA.
BACKGROUND:
Orchidometric evaluation of the testis has been proposed as a cost-effective alternative to measurement of the testis with high-frequency linear ultrasound, which may be costly in terms of hospital resources and patient time. It is known from animal experiments, autopsy series, and small clinical studies that under ideal conditions orchidometry may approximate ultrasound measurement. However, little is known of the effectiveness of orchidometry in the clinical setting in a large sample of adolescents with varicocele. We sought to analyze the performance characteristics of orchidometry and its agreement with ultrasound testis volumes in boys with varicocele.
METHODS:
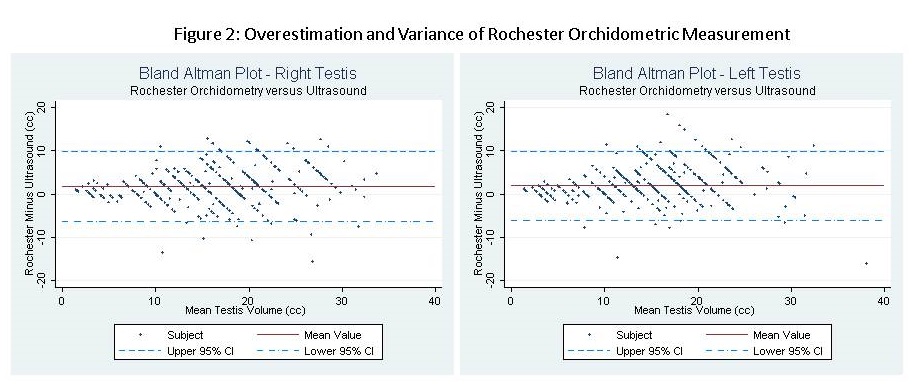
Our institutional varicocele database was analyzed from March 2000 to May 2013, including all boys with Rochester orchidometric measurement and ultrasound-based volume measurement performed on the same day. The Lambert formula (L*W*H*0.71) was used to calculate ultrasound volumes. 720 measurements were included: 360 of the left testis, and 360 of the right testis. Each subject was included once; in the event of serial measurements the earliest measurement was analyzed. Bland-Altman plots with 95% limits of agreement were used to compare orchidometry and ultrasound measurements. Analysis was performed with JMP®, v11 Pro. SAS Institute Inc., Cary, NC.
RESULTS:
Age at exam ranged from 11.2 - 18.5 years (mean 14.7). With respect to varicocele grade, 184 (51.1%) were grade III, 113 (31.4%) were grade II, 42 (11.7%) were grade I, 12 (0.3%) were bilateral and 11 (0.3%) were ungraded. Mean ultrasound left testis volume was 13.6 cc (SD 6.6) and mean right testis volume was 15.1 cc (SD 6.9). Eleven surgeons performed the measurements.
Mean overestimation on the right was 2.0 cc (SD 4.2) and on the left was 1.9 cc (SD 4.1); each was highly statistically significant (p<0.0001, paired t-test). Error was correlated with testis size, implying a greater degree of overestimation with increasing volume (p<0.01, Pearson’s correlation). Amount of volume overestimation and variability was not significantly different for right and left testis.
Sensitivity and specificity of Rochester orchidometry to detect a testis volume differential (TVD) of 20% were 33% (95% CI 23-42%) and 96% (95% CI 92-97%), respectively. In detecting 10% TVD, sensitivity and specificity were 52% and 86%. There was no effect on sensitivity or specificity of testis size, varicocele grade, or examining surgeon
CONCLUSIONS:
Appropriate caution should be exercised when relying solely on orchidometric evaluation of the testis. Rochester orchidometry in general appears to overestimate testis size, and there is wide variability in the estimation. In clinical practice, the sensitivity of Rochester orchidometry is modest in detecting a 20% testis volume difference; this difference would be missed in approximately 2/3 of boys screened with orchidometry alone.
Back to 2014 Fall Congress Meeting Abstracts
|

