-->
|
Back to 2014 Fall Congress Meeting Abstracts
BMI and Pediatric Urologic Surgical Complications: Results from Pediatric NSQIP
Michael P. Kurtz, MD MPH, Erin R. McNamara, MD, Anthony J. Schaeffer, MD MPH, Tanya Logvinenko, PhD, Caleb P. Nelson, MD MPH.
Boston Children's Hospital, Boston, MA, USA.
BACKGROUND: Elevated body mass index (BMI) is a well-known risk factor for perioperative complications in adults, but not in children undergoing urologic procedures. Given the low rate of complication associated with urologic surgery, a large sample is required, but BMI is frequently not available in large administrative databases. Here we report results from the first nationally-based prospectively-assembled cohort analyzed with respect to the influence of BMI on 30-day surgical complication for pediatric urologic procedures. We hypothesized that BMI would be associated with overall complication and wound complications.
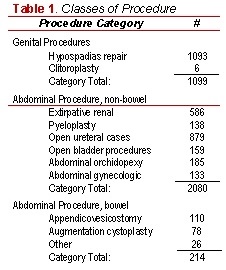
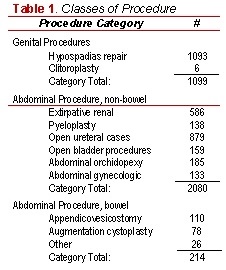
METHODS: We queried the 2012 Pediatric National Surgical Quality Improvement Program database (NSQIP), defining obesity as a BMI above the 95th percentile and overweight above the 85th percentile, per CDC definitions. We used BMI <85th percentile as a referent group. Complications were collected within 30 days of the procedure. Comorbidity was classified on a linear scale using a validated pediatric-specific comorbidity score, and procedures were classified as genital, abdominal without bowel involvement, or abdominal with bowel involvement (Table 1). Bivariate and multivariable logistic models were used to test significance of associations.
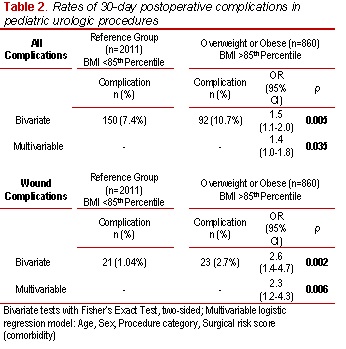
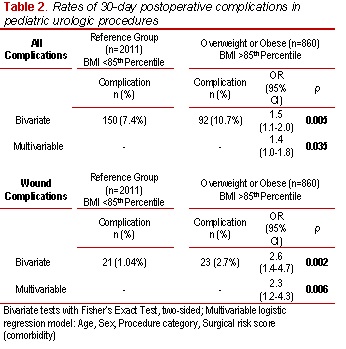
RESULTS: 2,871 patients aged 2-18 years were analyzed (Table 2). Of these, 420 (14.6%) were overweight and 440 (15.3%) were obese. Bivariate analysis revealed a 7.4% rate of complication in the reference group, 11.0% in overweight patients, and 10.5% in obese patients (p=0.013, Cochran Armitage trend test). On multivariable analysis adjusting for age, gender, class of procedure, and comorbidity, BMI remained a significant risk factor for complication when comparing obese/overweight patients to the reference population (p=0.035). An exploratory subgroup analysis examining the rate of wound complications demonstrated an odds ratio of 2.6 (95%CI 1.4-4.7, p=0.002) comparing obese/overweight patients to a referent range, which remained highly significant after adjustment for comorbidity, and case type (p=0.006).
CONCLUSION: BMI in the pediatric urologic population was found to be associated with overall complication after adjustment for case type and preoperative comorbidity in a large national sample assembled for assessment of perioperative outcomes. An exploratory analysis uncovered more than two-fold odds of wound complication in obese/overweight patients compared to a normal weight referent population. These results may be useful in preoperative counseling patients regarding perioperative risk.
Back to 2014 Fall Congress Meeting Abstracts
|