-->
|
Back to 2014 Fall Congress Meeting Abstracts
30-Day Morbidity After Augmentation Enterocystoplasty and Appendicovesicostomy: A NSQIPP Analysis
Erin R. McNamara, MD, Michael P. Kurtz, MD MPH, Anthony J. Schaeffer, MD MPH, Tanya Logvinenko, PhD, Caleb P. Nelson, MD MPH.
Boston Children's Hospital, Boston, MA, USA.
Background: Although reconstructive procedures such as augmentation enterocystoplasty (AC) and appendicovesicostomy (AV) are among the most complex procedures in pediatric urology, with high potential morbidity, there are few data regarding the incidence of post-operative complications after AC/AV, especially from a large national sample. Our objective was to describe and evaluate predictors of 30-day morbidity and complications in a national multi-institutional prospective database.
Methods: Using the American College of Surgeons-National Surgeon Quality Improvement Program Pediatric (ACS-NSQIPP) database, we reviewed all patients undergoing AC and /or AV in 2012. ACS-NSQIPP collects data on 327 variables, including perioperative data, postoperative complications, reoperation and readmissions after major surgical procedures at 50 participating sites. Complications within 30 days of the procedure were reviewed and predictors of any 30-day event (complication, readmission, reoperation) were identified using multivariable logistic regression. Comorbidity was assessed using the surgical risk score, a validated multispecialty index.
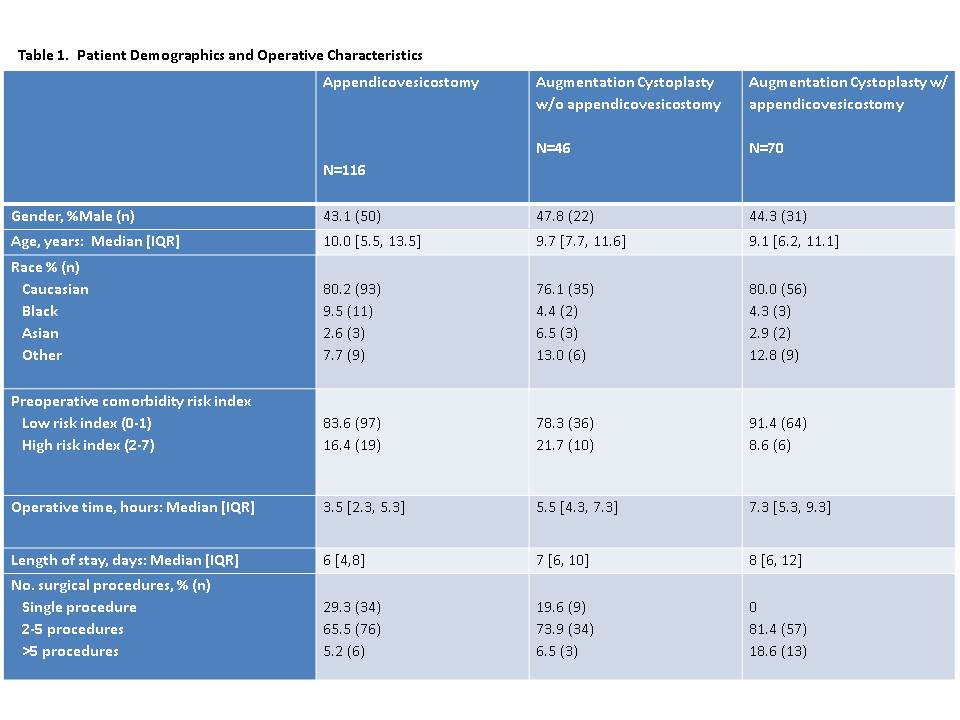
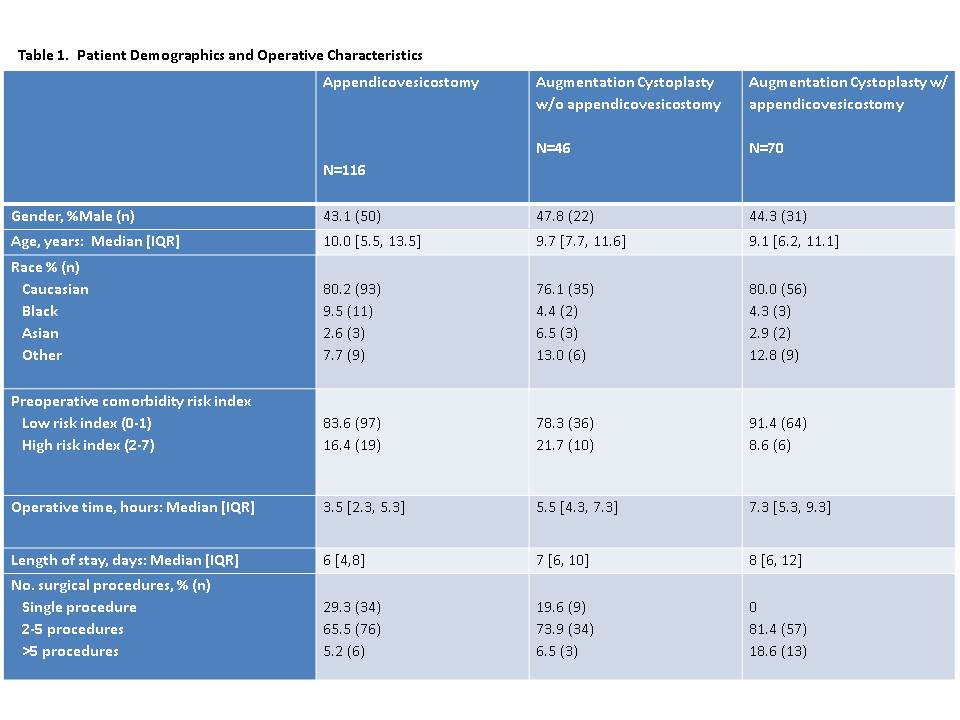
Results: There were 232 patients identified: 116 had AV, 46 had AC, and 70 had both procedures. The primary diagnosis listed was neurogenic bladder/bowel or spina bifida in 161, urinary incontinence in 14, bladder exstrophy in 14, other urinary diagnoses in 29, malignancy in 2, renal failure in 1 and unknown in 11. Patient demographics and operative characteristics are shown in Table 1. 30-day outcomes are shown in Table 2. 43/232 (18.5%) patients had postoperative complications. UTI was the most common postoperative complication, seen in 9.5% of all patients, with wound complications in 7.8%, bleeding in 3.4% and sepsis in 2.2%. Of those that had complications, 10/43 (23.3%) had more than one complication. 31/232 (13.4 %) were readmitted within 30 days of surgery, with median time to readmission of 18 days [IQR 11-26]. Reasons for readmission included UTI, wound complications, other urinary issues, bowel issues, C. Difficile infection, thromboembolic disease, and malfunctioning or infected GU devices. Unplanned reoperation was seen in 20/232 (8.6%) patients. Any 30-day event (complication, readmission, or reoperation) occurred in 68/232 (29.3%) patients. On multivariable analysis, when controlling for age, gender, and type of operation, both higher surgical risk score (OR: 2.2, 95%CI 1.1-4.8, p=0.04) and longer operative time (OR: 1.2, 95%CI 1.1-1.3, p=0.002) were associated with incidence of any 30-day event.
Conclusions: After AC and/or AV, significant adverse events are common, including readmission and reoperation. Patients at higher risk of adverse events can be identified by preoperative risk scores, and among those with longer operative times. Future research should seek to identify and mitigate the sources of morbidity after these high-risk procedures.
Back to 2014 Fall Congress Meeting Abstracts
|