-->
|
Back to 2014 Fall Congress Meeting Abstracts
Mucosal inflammation rapidly alters urothelial keratin 6 and 14 expression promoting a skin-like phenotype
Christina B. Ching, MD1, David J. Degraff, PhD2, Matthew D. Mason, MD1, Magdalena M. Grabowska, PhD1, Peter E. Clark, MD1, Simon W. Hayward, PhD1, Robert J. Matusik, PhD1, Philip Owens, PhD1, John C. Thomas, MD1, Stacy T. Tanaka, MD1, John C. Pope, IV, MD1, Mark C. Adams, MD1, John W. Brock, III, MD1, Douglass B. Clayton, MD1.
1Vanderbilt University, Nashville, TN, USA, 2Penn State Hershey, Hershey, PA, USA.
Mucosal inflammation rapidly alters urothelial keratin 6 and 14 expression promoting a skin-like phenotype
Introduction:
Alterations in urothelial keratin (Krt) expression are associated with chronic mucosal inflammation, most notably with chronic indwelling catheters; such alterations help characterize squamous metaplasia and squamous cell carcinoma of the bladder. Krt 6 and Krt 14 are both expressed abundantly in skin but have very limited expression in the normal human or mouse bladder. We hypothesized that mucosal inflammation in the mouse bladder would alter keratin expression prior to the development of squamous phenotypes.
Materials and Methods:
Female C57B6 mice were subjected to one of several benign bladder injury models, including partial bladder outlet obstruction, acute bladder overdistention, repeated bladder overdistention, or acute intravesical lipopolysaccharide administration. All mice underwent oophorectomy one week prior to injury to minimize the variability of inflammation due to estrogen flux. All injury models used in the experiments have been previously described. At various time points after injury, bladder tissue specimens were excised and fixed in 10% formalin. Paraffin-embedded sections were immunostained using a panel of urothelial markers including Uroplakin 2, FoxA1, Ki67, and Keratins 5, 6, and 14.
Results:
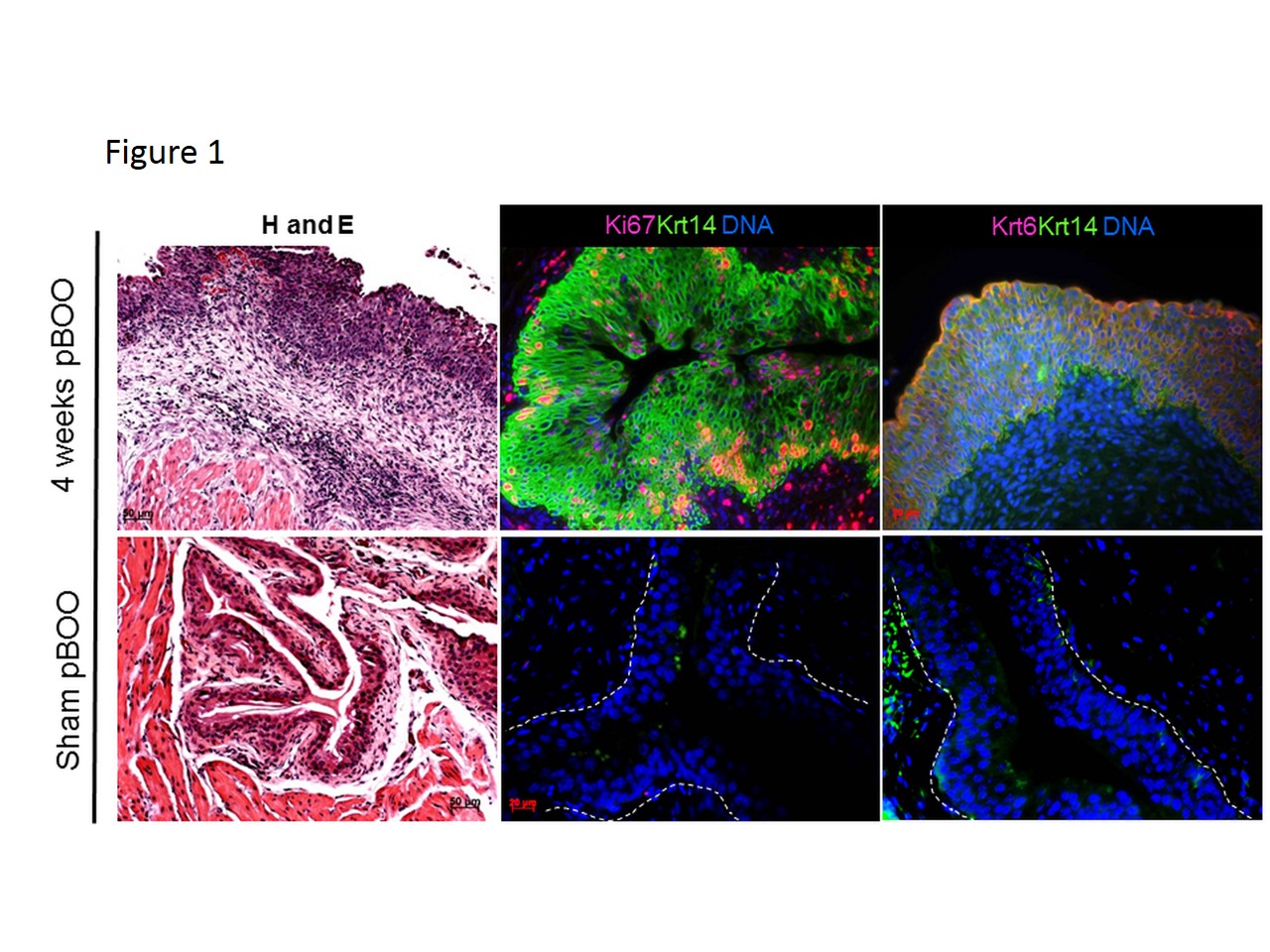
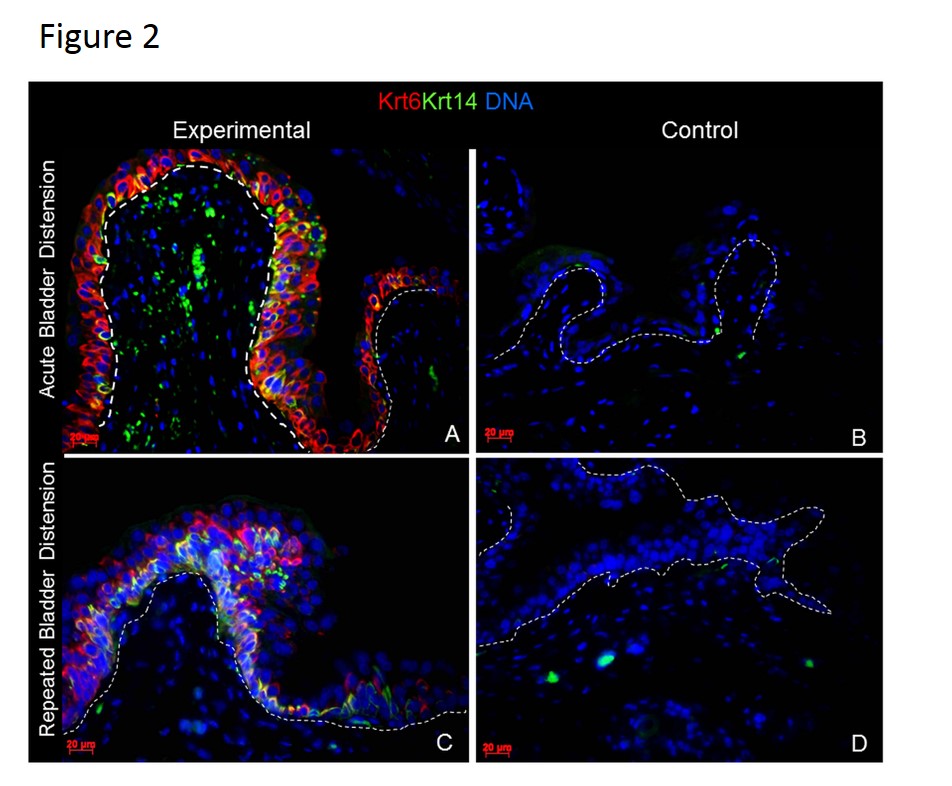
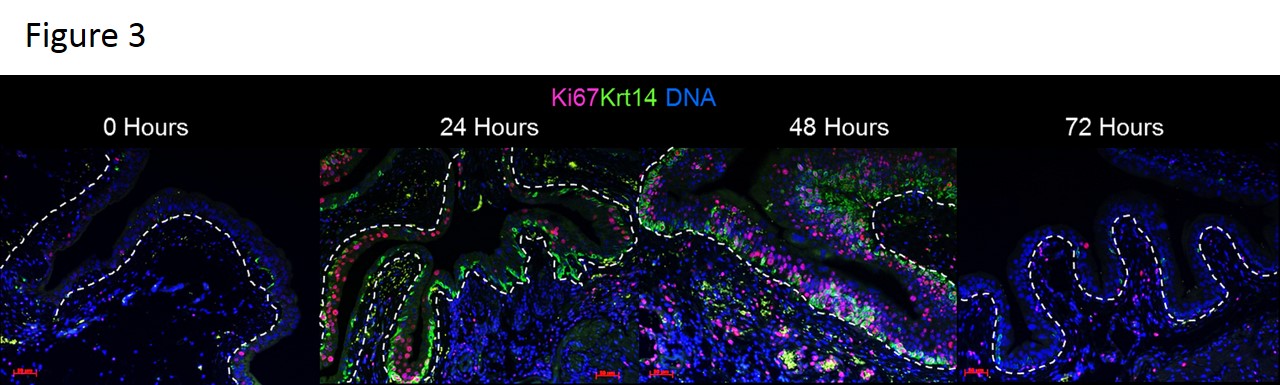
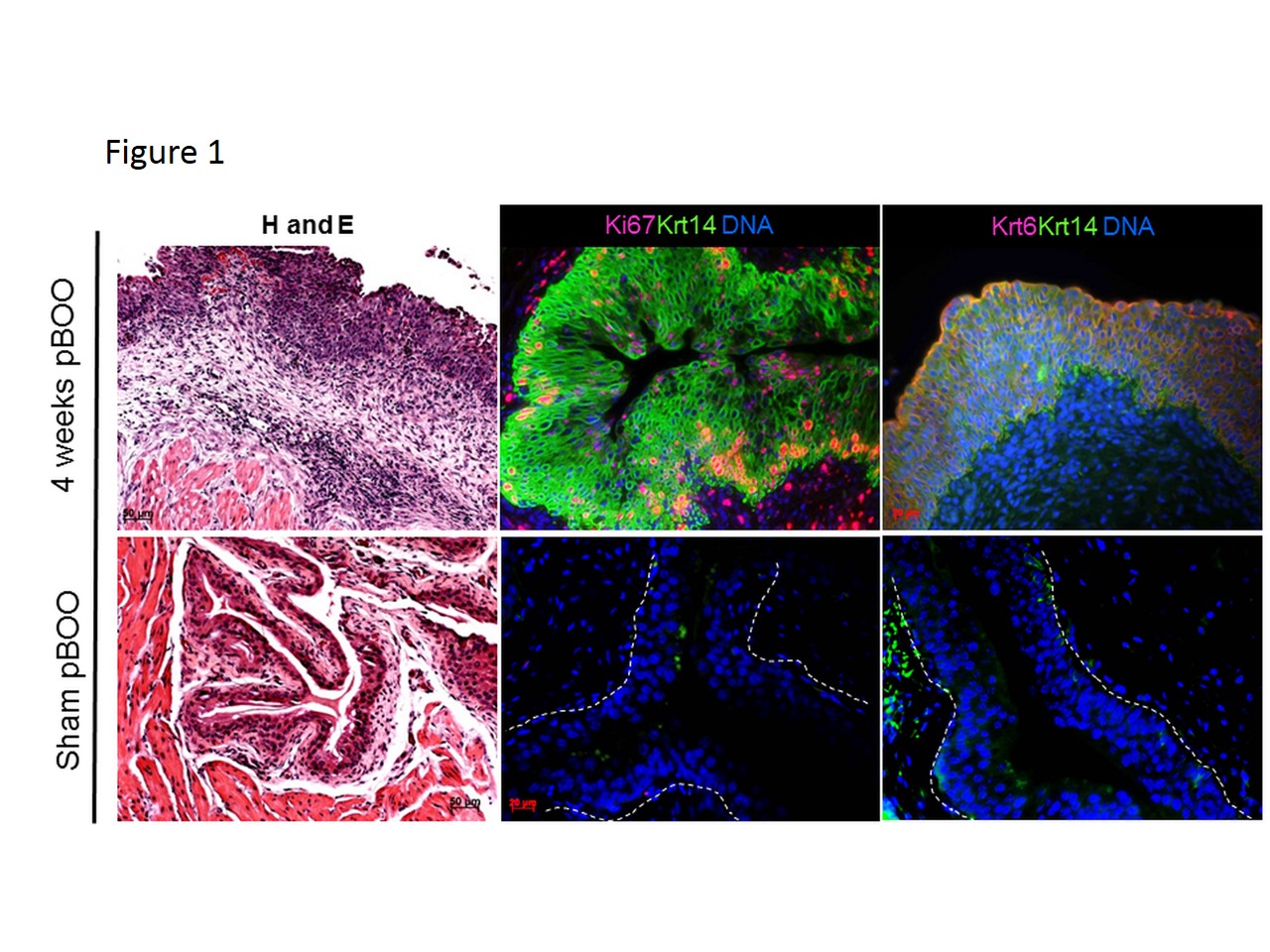
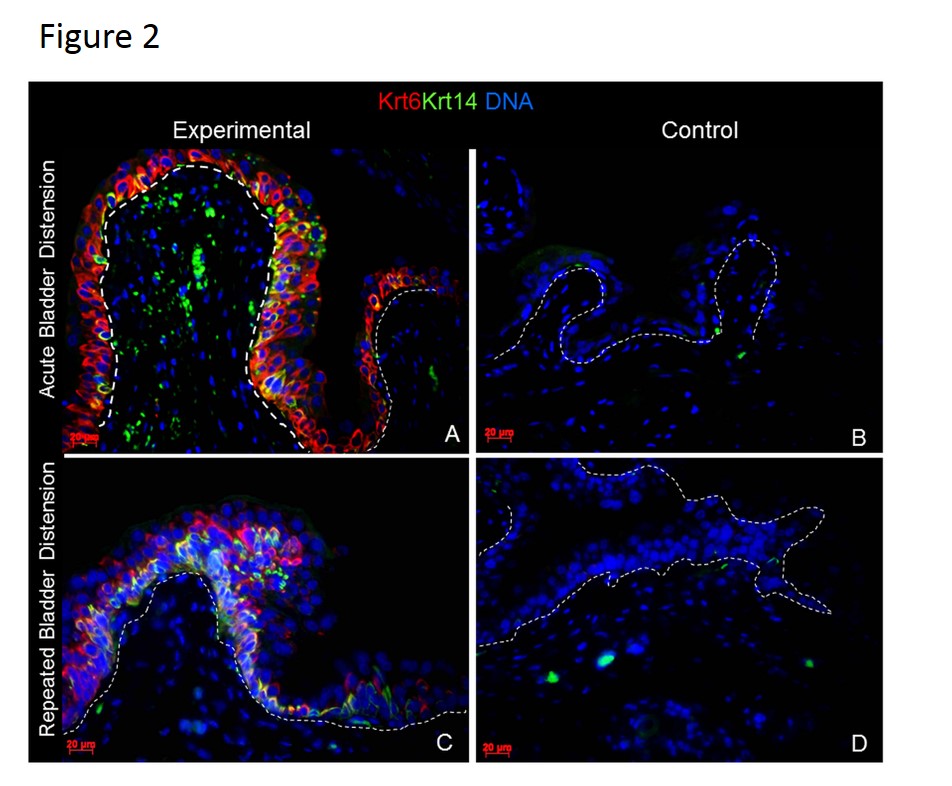
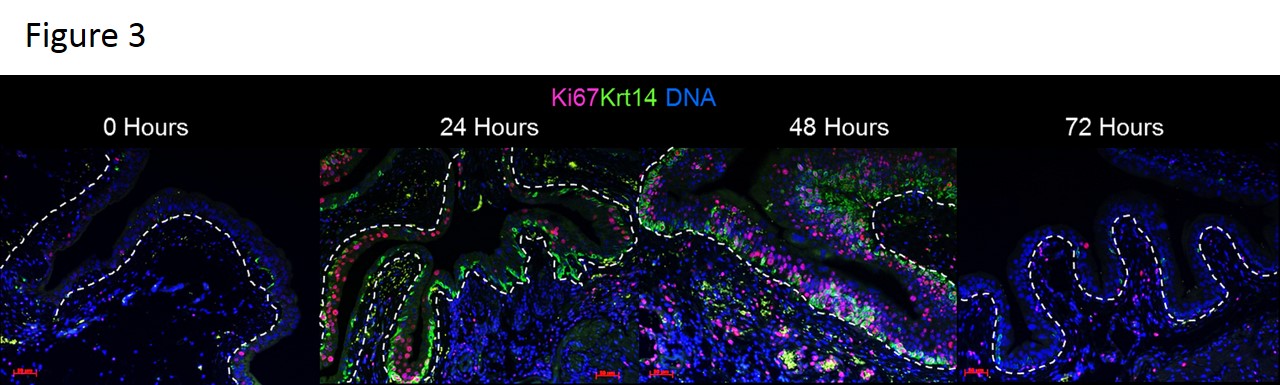
In the normal mouse bladder, Krt 5 is a constitutive marker of the basal urothelium while Krt 6 and Krt 14 are expressed only in rare urothelial cells along the basement membrane. At various time points after induction of partial bladder outlet obstruction (2, 4 and 13 weeks), mucosal inflammation was associated with a dramatic expansion of Krt 5, 6, and Krt 14 expression urothelial cells as compared to sham animals (Figure 1). We then utilized acute injury models to examine the kinetics of these keratin changes. Interestingly, urothelial expression of Krt 6 and Krt 14 was rapidly altered by mucosal inflammation 24 hours after a single bladder overdistension and after 5 days of repetitive bladder overdistension (Figure 2). Additionally, similar Krt changes were seen 24 hours after a single intravesical LPS administration (not shown). Time course analysis of animals undergoing acute bladder overdistension demonstrated rapid increases in Krt 6 and Krt 14 expression by 24 hours and rapid decreases in these proteins as inflammation resolved by 72 hours (Figure 3).
Conclusion:
Up to the present, changes in Krt expression have been specifically associated with squamous phenotypes and with squamous cell carcinoma. In this work, we show that changes in Krt expression are part of a conserved program of urothelial response to mucosal inflammation and that stressed urothelium exhibits protein patterns similar to skin. Finally, Krt changes occur quickly and well in advance of squamous phenotypes.
Back to 2014 Fall Congress Meeting Abstracts
|