-->
|
Back to 2014 Fall Congress Meeting Abstracts
Hospital Admissions for Initial Febrile Urinary Tract Infection in the Era of Revised American Academy of Pediatrics UTI Guidelines: Do Patient Demographics Matter?
Angela M. Arlen, MD1, Laura S. Merriman, MD1, Traci Leong, PhD2, Kristin M. Broderick, MD1, Hal C. Scherz, MD, FAAP, FACS1, Edwin A. Smith, MD, FAAP, FACS1, Bruce H. Broecker, MD, FAAP, FACS1, Andrew J. Kirsch, MD, FAAP, FACS1.
1Emory University/Children's Healthcare of Atlanta, Atlanta, GA, USA, 2Emory University College of Public Health, Atlanta, GA, USA.
Background
In 2011, the AAP revised their practice parameters regarding febrile urinary tract infection (fUTI) in children aged 2-24 months. In their response to these new guidelines, the Section of Urology expressed concern that the impact of this recommendation may be particularly felt among financially disadvantaged children. We evaluated young children presenting to the emergency room setting with initial fUTI to determine predictors of hospital admission.
Methods
Two cohorts of children, aged 2 to 24 months, were assessed in the emergency department setting over two separate six-month periods - from January to June 2011 and January to June 2012 - to evaluate effect of the guidelines. Patient demographics, insurance status, fever, urine culture, laboratory studies, renal/bladder ultrasound (RBUS), VCUG and admission status were evaluated. The relationship between admission status and both continuous and categorical variables was assessed using a logistic regression model. Insurance status of clinic patients with fUTI or VUR was also determined. Children with previous history of VUR or VCUG, prior fUTI, undocumented urine culture or afebrile UTI (temperature <101.5 ° F) were excluded.
Results
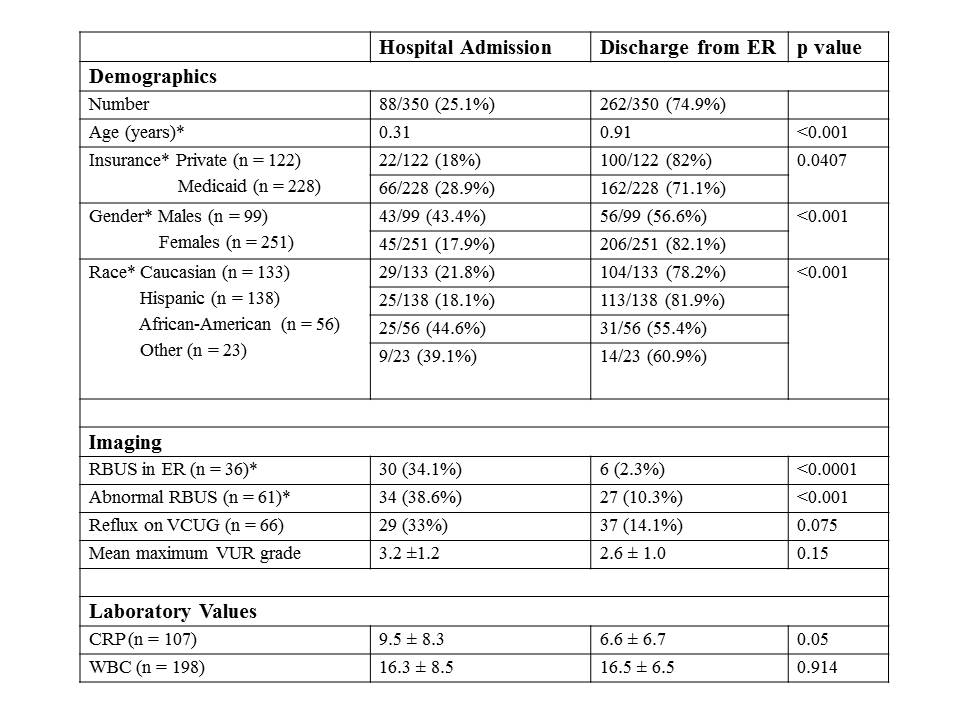
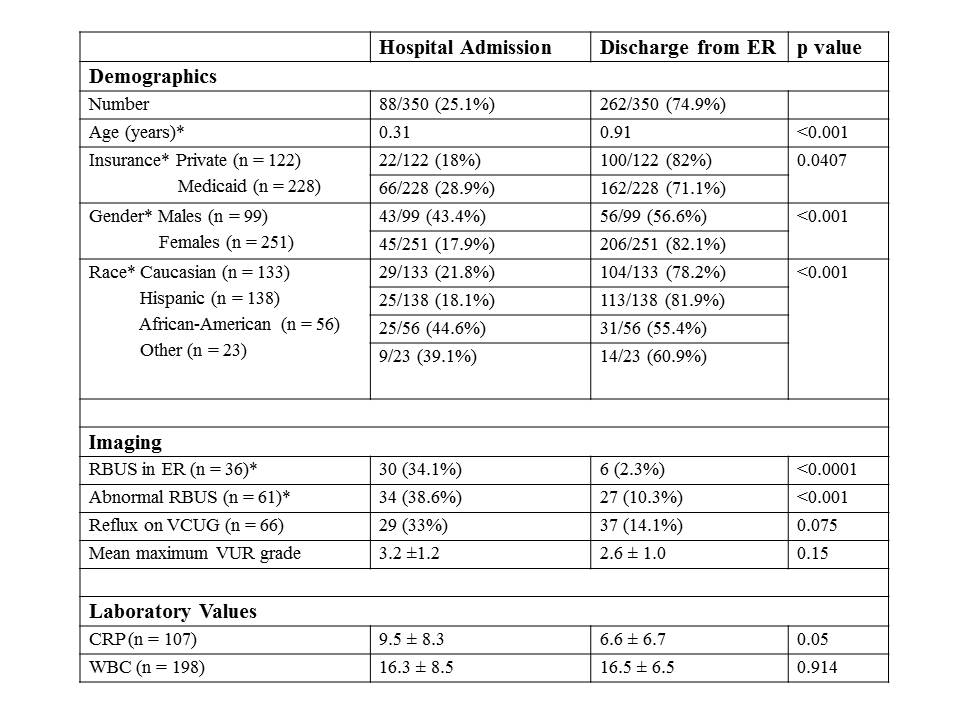
In 2011, 172 patients presented with initial fUTI and 47 children (27.3%) required hospitalization. In 2012, 41 (23.1%) of 178 patients were admitted. Admission by year was not significantly different (p = 0.423). Results of univariate analysis are summarized in the Table. Patients requiring admission were significantly (p<0.001) younger (mean age 0.31 ± 0.33 years) than those managed as outpatients (mean age 0.91 ± 0.7 years). The number of admitted females was similar to males, however there were 251 females compared to 99 males (2.54:1). Male gender was therefore associated with significantly higher likelihood of admission (p<0.001). Children with abnormal RBUS were significantly more likely to have required admission than those with a normal RBUS (p<0.001). C-reactive protein was marginally significant between admitted children (mean 9.5 mg/dL) and those discharged from the ER (mean 6.6 mg/dL; p = 0.05). Abnormal RBUS retained significance on multivariate analysis. Children with abnormal RBUS were 12.8 times more likely to require hospital admission (95% CI, 4.44-37.0). Medicaid was an independent predictor of hospital admission on multivariate analysis; such patients were 2.6 times more likely to be admitted than private insurance patients (95% CI, 1.15-5.88). During the same time interval, only 44.2% of children presenting to the outpatient clinic with similar diagnoses had Medicaid, compared to 65.1% of those presenting to the ER (p<0.0001).
Conclusions
Children presenting to the ER setting with fUTI may be more ill, more likely to require hospitalization, and more likely to have Medicaid than those managed in an outpatient clinic. Abnormal RBUS, race and Medicaid were all strongly associated with hospital admission regardless of year. As children with government sponsored healthcare are less likely to have a usual primary care provider, there remains significant medico-economic concern regarding the broad application of the new AAP UTI guidelines.
Back to 2014 Fall Congress Meeting Abstracts
|