-->
|
Back to 2014 Fall Congress Meeting Posters
Assessment of the Unplanned Post-operative Morbidity in Children (UPMC) Scoring System for use in Pediatric Urology
Moira E. Dwyer, M.D., Heidi A. Stephany, M.D., Glenn M. Cannon, Jr., M.D., Steven G. Docimo, M.D., Francis X. Schneck, M.D., Omaya Banihani, M.D., Michael C. Ost, M.D..
Children's Hospital of Pittsburgh of the University of Pittsburgh Medical Center, Pittsburgh, PA, USA.
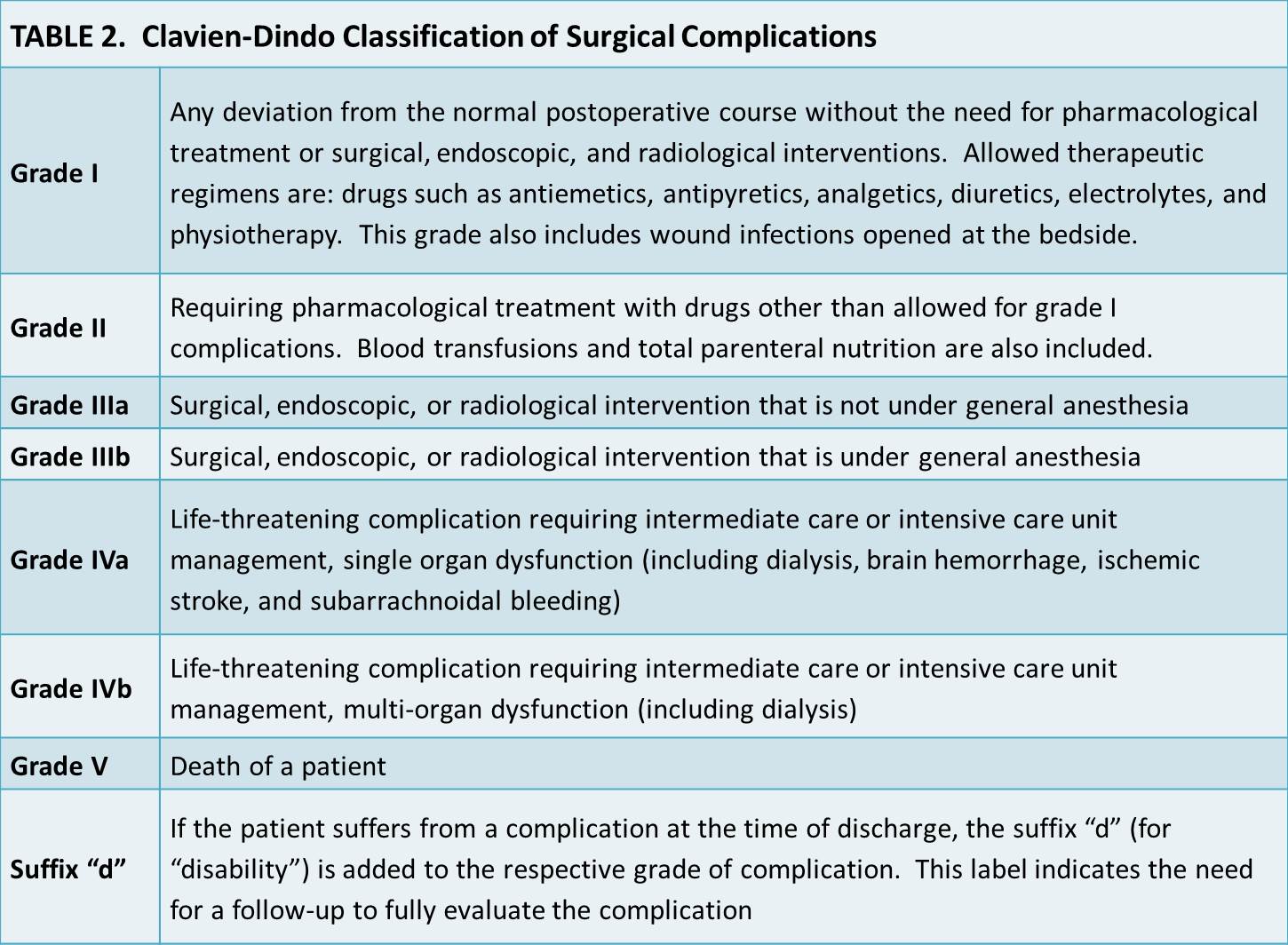
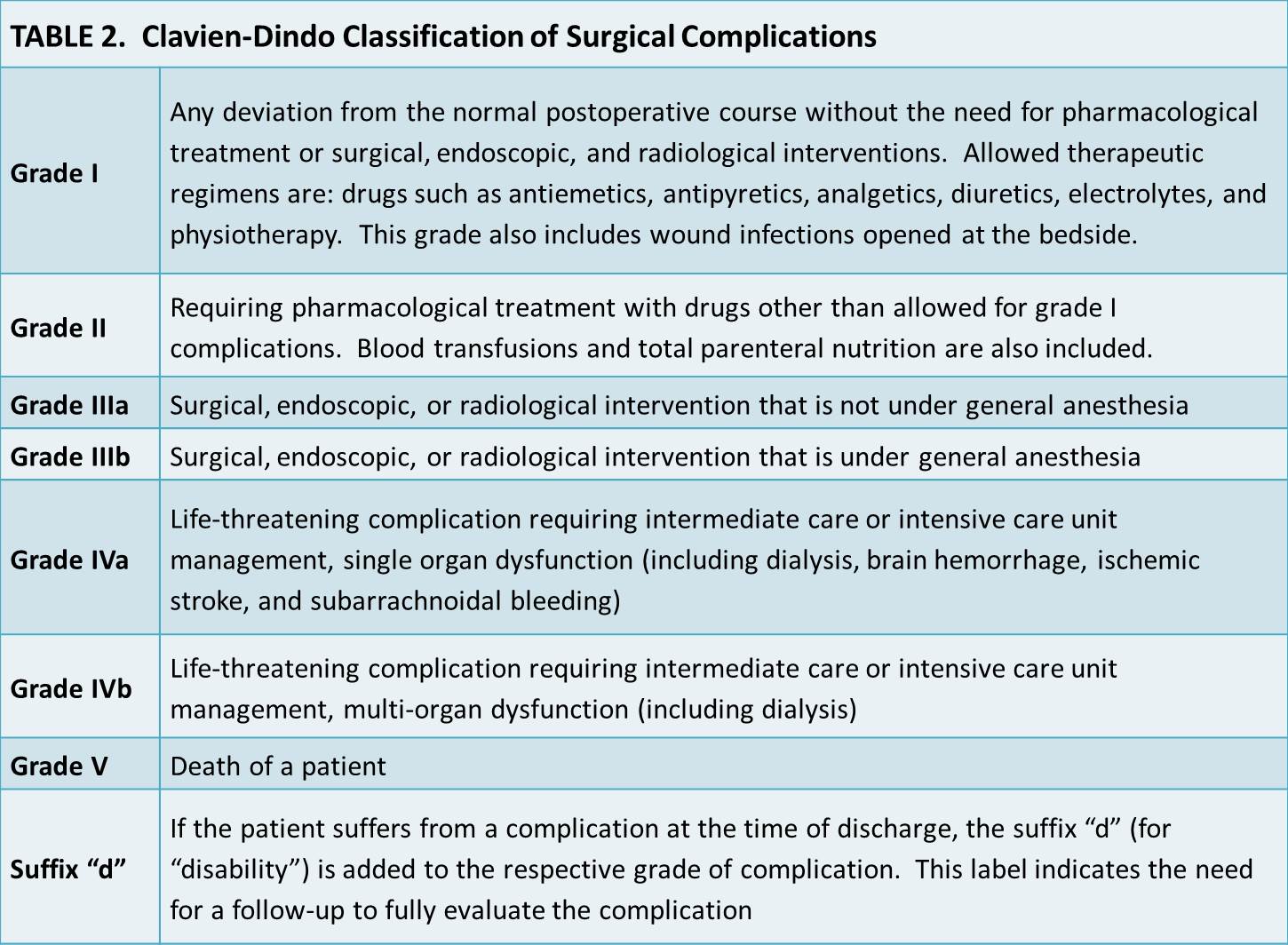
BACKGROUND: Although use of the Clavien-Dindo Classification of Surgical Complications is becoming more widespread within urology, this system was developed using a cohort of 6,336 adult general surgery patients. We proposed a novel Unplanned Post-operative Morbidity in Children (UPMC) scoring system to capture the global morbidity of unexpected post-surgical events on the child through surrogates for pain, traumatic experiences, and time away from home/school environments while accounting for the negative impacts of radiation exposure, general anesthesia, and short-term/lasting disabilities (Table 1). We set out to evaluate the acceptability and reproducibility of this system and compare it to the Clavien-Dindo system (Table 2) for use in pediatric urology.
METHODS: Replicating the methods of Dindo, Demartines, and Clavien, we used the “Survey to Assess Acceptability and Reproducibility of the Classification” that had been sent to heads or senior surgeons of ten surgical departments with the request to distribute the survey to surgeons and trainees. For Questionnaire 1, we replaced the 14 adult surgical cases with 14 pediatric urology cases of the same Clavien-Dindo grade except for an additional disability suffix in two cases. We added to Questionnaire 2 questions about the applicability of the classification systems to pediatrics and respondent demographics. We used REDCap electronic data capture tool to send the survey to 29 Pediatric Urology Fellowship Program Directors with a request to distribute to other pediatric urologists and trainees including the information for determining the Clavien-Dindo and UPMC Classifications. Replies were anonymous.
RESULTS: We received 20 complete survey responses and 10 partial responses. All 20 (100%) indicated that they think the UPMC scoring system is appropriate for pediatrics and also that it respects patient and hospital perspectives versus 50% (10/20; p=0.0004) and 63% (12/19; p=0.003), respectively, for the Clavien-Dindo system. There was a significantly lower percentage of correct class assignment for the 14 cases with the Clavien-Dindo system (79%, 229/291) versus the UPMC scoring system (88%, 247/282; p<0.0001), which had a percentage that did not significantly differ from that which was accepted in the original assessment of the Clavien-Dindo system (90%, 1816/2016; p=0.21). However, the intercoder reliability was poor for the UPMC raw score (0.372), class (0.342), and death classification (0.120) (0.667=minimum acceptable level of agreement, 0.800=good agreement, and 1.000=perfect agreement). Also, half of respondents (10/20) did not think the UPMC scoring system was simple whereas only 10% held this perception of the Clavien-Dindo system (2/20; p=0.01).
CONCLUSIONS: While the proposed UPMC scoring system is uniformly perceived as appropriate for pediatrics and is superior to the Clavien-Dindo system for accurate classification of morbidity in pediatric urology patients, it lacks intercoder reliability. Efforts should be made to develop a system that is appropriate as well as user-friendly with good intercoder reliability.
Back to 2014 Fall Congress Meeting Posters
|