-->
|
Back to 2014 Fall Congress Meeting Posters
Urethrocutaneous Fistula Formation in Children undergoing Hypospadias Repair under Caudal Anesthesia versus Penile Block
Nina Casanova, MD, Raza Zaidi, MD, Adam Eickmeyer, BS, Tabitha Kalabat, none, Terri Voepel-Lewis, PhD, Bishr Haydar, MD, Julian Wan, MD.
University of Michigan, Ann Arbor, MI, USA.
BACKGROUND: Urethrocutaneous fistula is a well-known complication of hypospadias surgery. Fistulae are most often due to distal obstruction and poor vascular tissue coverage. A recent prospective study by Kundra et al. has suggested that caudal anesthesia may also increase the risk of fistula formation. Given the common use of regional blocks for penile surgery, we sought to confirm or refute this possible association and to determine if any other novel factors may be associated with increased fistula formation.
METHODS: Children who underwent primary hypospadias repair performed by a fellowship trained pediatric urologist between January 1, 1994 and March 31, 2013 at our tertiary care center were included in this retrospective, nested case-controlled study. All cases of fistulae were identified by independent review of multiple repairs, and the diagnosis was validated by a secondary review. Two matches for every case were randomly selected from the remaining list as controls. Children with multi-stage repair, connective tissue and bleeding disorder were excluded. Reviewed data included: age, medical history, social demographics (assessed by zip code), details regarding caudal anesthesia, penile block, use of subcutaneous epinephrine, location of the urethral opening, type of repair, other surgical factors, recovery characteristics, postoperative infection and outcomes. Chi square or Kruskal Wallis tests were used to evaluate the association between various perioperative factors and fistula occurrence.
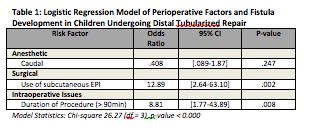
RESULTS: Forty-five cases and ninety controls were reviewed. Fistula occurrence was not significantly associated with anesthetic type, postoperative pain assessments, or surgeon experience (years since training completion) on univariate analyses. Conversely, the location of the urethral opening (distal vs. midshaft/proximal), duration of the procedure, as well as the use of subcutaneous epinephrine were strongly associated with fistula formation. On multivariate analysis, only the distal tubularized repairs were evaluated to standardize the cohort and those results are listed in Table 1. As assessed by zip code, the distance from patient home to the surgical center (> or ≤2 hours), median income (≥ or < national average), and quartiles for healthcare outcomes were also independent of fistula rates (p=0.44, p=1.0, and p=0.70 respectively).
CONCLUSIONS: The use of regional anesthetic in children undergoing primary hypospadias repair was not associated with urethrocutaneous fistula formation. Location of the urethral opening appears to be strongly associated with fistula development (proximal > midshaft > distal) as previously described in the literature. Subcutaneous epinephrine use was also associated with fistula formation. Its vasoconstrictive properties may help with hemostasis but jeopardize tissue healing and calls into question its routine use. Travel distance from home to a tertiary surgical “center of excellence” and socioeconomic factors such as median income and health care quartiles were not significant factors. This suggests that tertiary care involving technical interventions, such as hypospadias repair, can effectively be carried out despite long distances and wide variations in local health care quality.
Back to 2014 Fall Congress Meeting Posters
|