-->
|
Back to 2014 Fall Congress Meeting Posters
Differences in Patient Comprehension and Communication Effectiveness using In-Person and Telephonic Medical Interpretation Services
David J. Chalmers, MD1, Austine K. Siomos, MD1, Michael Bronsert, PhD2, Vijaya M. Vemulakonda, MD JD1.
1Children's Hospital Colorado, Aurora, CO, USA, 2University of Colorado School of Medicine, Aurora, CO, USA.
Background: Language barriers between providers and patients with limited English proficiency (LEP) diminish understanding and adherence to follow up instruction. While the use of trained interpreters is thought to mitigate this problem, the optimal mode of medical interpretation is unknown. We hypothesized that telephone and in-person interpretation for Spanish-speaking LEP families and their respective providers differ in provider perceived communication effectiveness and parental comprehension of their child’s medical condition.
Materials and Methods: Consecutive Spanish-speaking families seen at the Children's Hospital Colorado main campus in two outpatient clinics (Pediatric Urology, Pediatric Cardiology) from September, 2013 through April, 2014 were included. The study was conducted as a quality improvement project (ORRQIRP #1308-7) and not deemed under the purview of IRB approval. Patients were excluded if communication was conducted in English or a language other than Spanish, or if interpretation was facilitated by other means, such as a Spanish-speaking provider or an English-speaking family member. Families who utilized an in-person or telephone interpreter completed questionnaires following their appointment. Comprehension of the medical problem was assessed by open ended questions regarding diagnosis, treatment plan, medications and alternative surgical options. Responses were compared to provider responses and rated as “accurate” vs “inaccurate”. Non-responses were also recorded. Additionally, providers completed questions assessing delays in appointments and barriers to communication. Differences in responses and response accuracy were compared by χ2 tests.
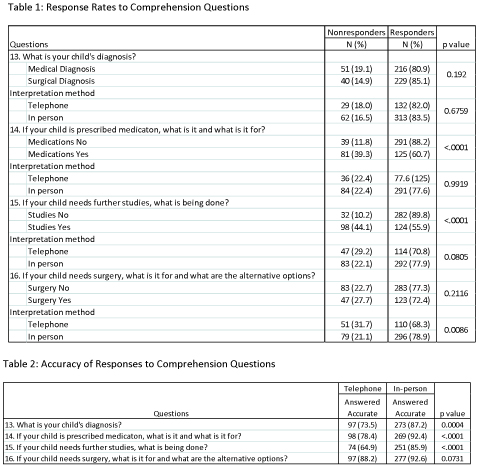
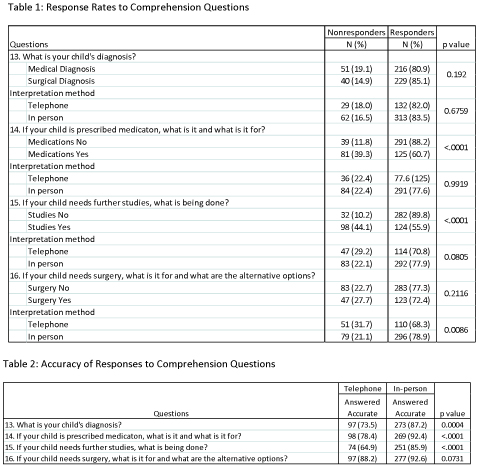
Results: 536 patients met inclusion criteria (161 telephone vs 375 in-person interviews). Parental response rates to comprehension questions ranged from 55.5% to 88.2% and were greater with in-person interpretation (Table 1). Families responded with significantly greater accuracy to all questions with in-person interpretation (Table 2). Providers recorded appointment delays with greater frequency when an in-person interpreter was used (24.0% vs 11.8%, p=0.0013) and recorded prolonged interviews and impeded communication more frequently with telephone interpretation (42.9% vs 1.3%, p<0.001 and 40.4% vs 1.3%, p<0.001 respectively). Response rate and accuracy to all questions significantly decreased when providers reported communication barriers (Table 3).
Conclusions: Significant differences exist between in-person and telephone interpretation for Spanish-speaking LEP families. While the use of in-person interpreters led to more appointment delays, communication effectiveness was perceived to be significantly better than telephone interpretation. Furthermore, provider impression of higher communication effectiveness is associated with improved parental comprehension their child’s medical condition.
Back to 2014 Fall Congress Meeting Posters
|