-->
|
Back to 2014 Fall Congress Meeting Posters
DISTAL URETEROURETEROSTOMY FOR REPAIR OF UPPER-POLE ECTOPIC URETER IN CHILDREN: IS STENTING REALLY NECESSARY?
Luis Braga, MD, MSc, PhD, David M. Kanters, BSc, MSc, Jorge DeMaria, MD.
McMaster University, Hamilton, ON, Canada.
BACKGROUND:
Duplex systems with upper-pole ectopic ureters may be associated with an increased incidence of UTI, urinary incontinence, renal obstruction, and VUR. Surgical management is aimed at reducing these complications and preserving upper-pole renal function. Distal ureteroureterostomy (U-U) is a minimally-invasive option and can be performed with or without a stent. Our goal is to report a prospective analysis with this technique and compare the outcomes of stented vs. stentless U-U.
METHODS:
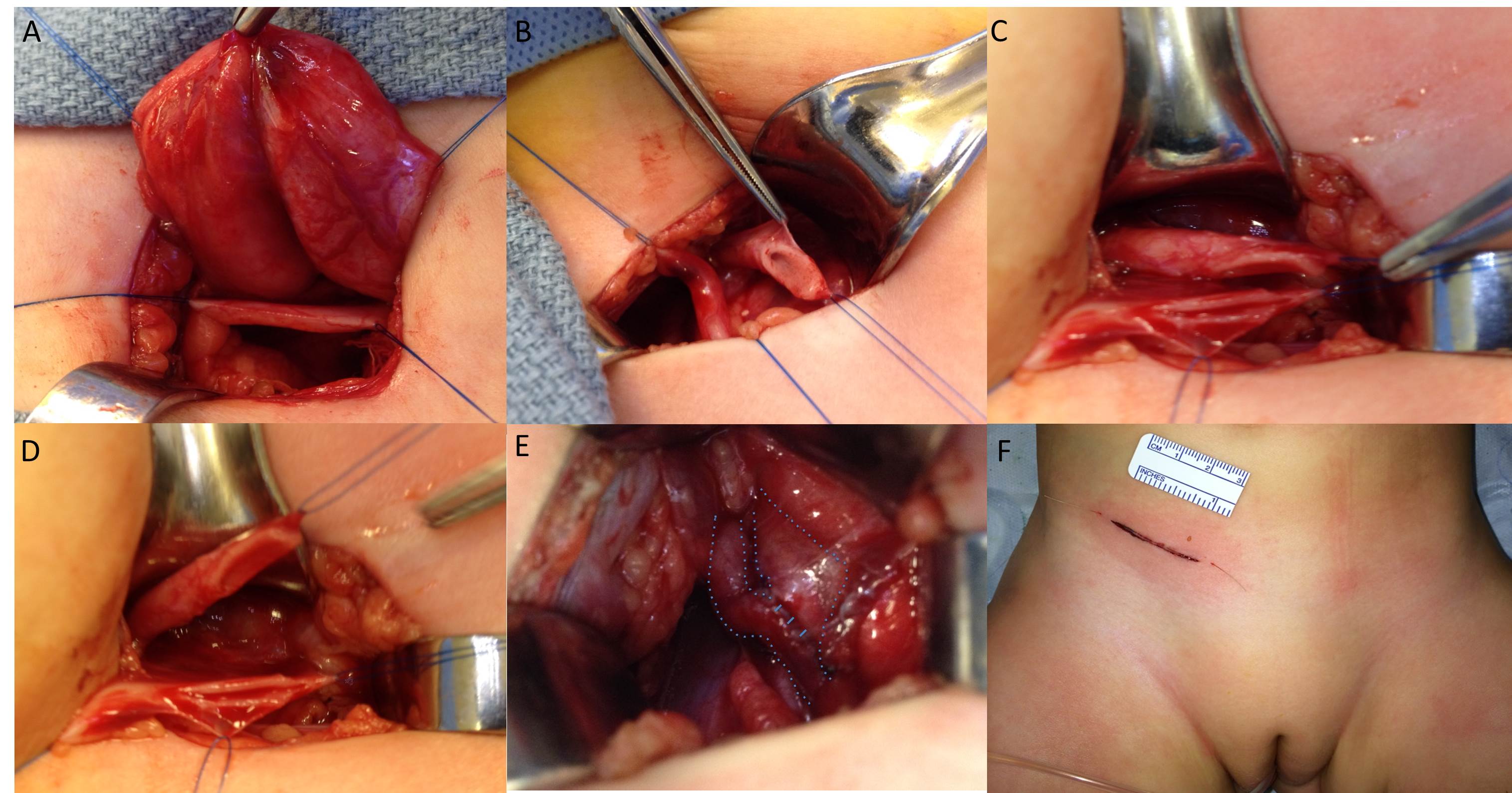
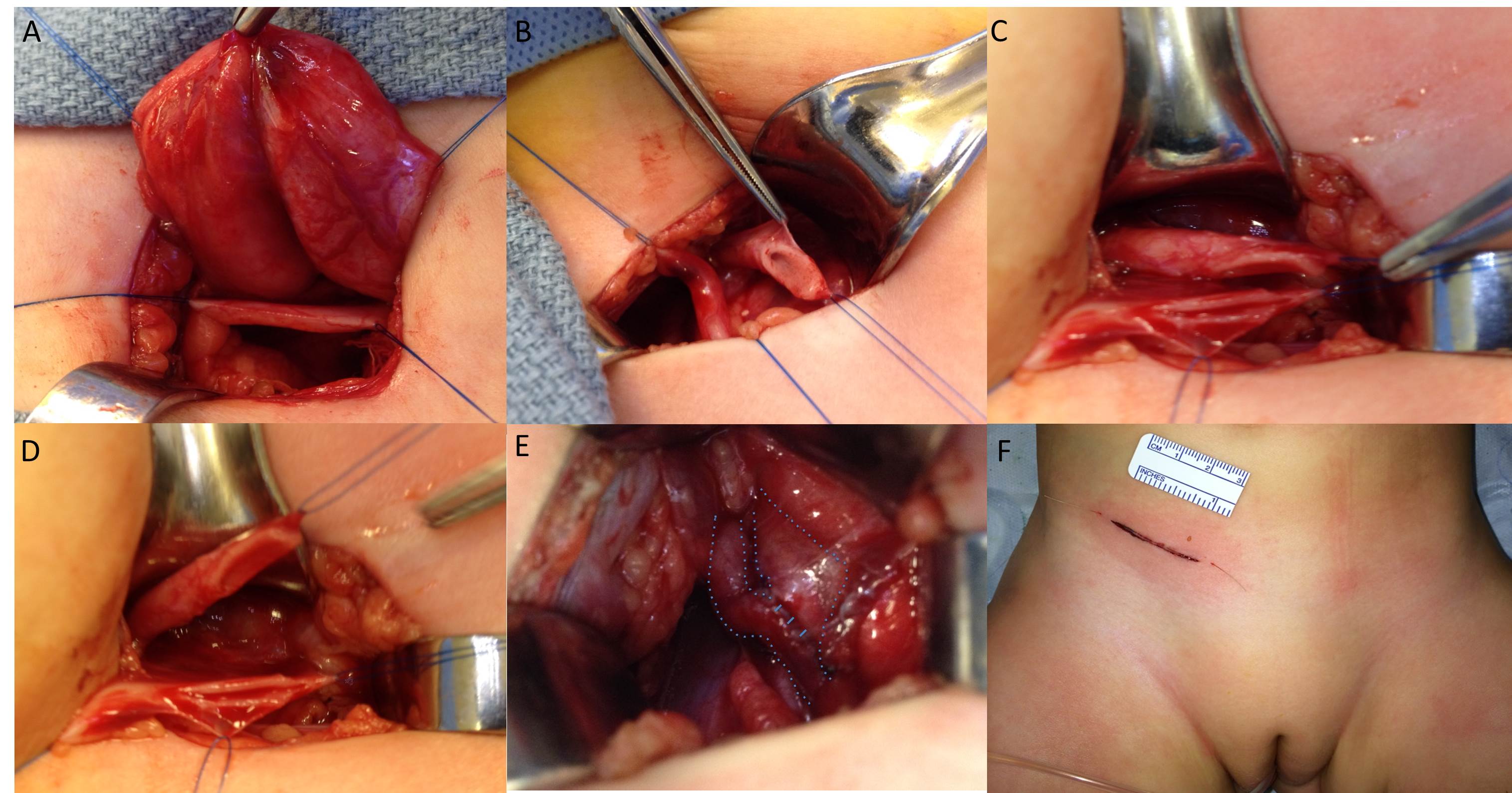
From 2009-14, all children who underwent U-U for upper-pole ectopic ureters and no VUR were prospectively followed. Age at surgery, gender, follow-up duration, presentation of ectopic ureter, hydronephrosis SFU grade, upper-pole renal function, ectopic ureter location, use of stent, ureteric caliber, operative time, and hospital stay were recorded. Complications and time to resolution of hydroureteronephrosis (defined as SFU grade I or 0 at last F/U) were assessed. Upper-pole renal function was determined by renal scan/doppler ultrasound. One surgeon stented all anastamoses whereas the other did not based on their routine practice, without any selection bias. All cases were performed through a small transverse inguinal incision (Figure). Student’s t-and Fisher’s Exact tests were used to compare complication rates.
RESULTS:
U-U was performed on 47 patients with a median age at surgery of 6 mos (1-72). Nineteen (40%) were male and 28 (60%) female. Median F/U was 14 mos (4-32). Presentation included UTI in 9 (19%), antenatal diagnosis in 37 (79%), and urinary incontinence in 1 (2%). Of the 47 patients, 33 (70%) had Grade III SFU hydronephrosis and 14 (30%) Grade IV. Upper-pole renal function was preserved in 39 (83%) children. Mean preoperative ureteric dilation was 15.3±3.29mm. In 19 boys, ectopic ureter was located at the bladder neck in 7 (37%) or posterior urethra in 12 (63%). In 28 females, ectopic ureter location was at the bladder neck in 14 (50%), posterior urethra in 9 (32%), or vagina in 5 (18%). Stentless U-U was performed 17 (36%) patients and 30 (64%) were stented. Mean operative time was 90 ±14.2 min. Median postoperative hospital stay was 24 hours (12-36). Postoperatively, 6 of 30 patients with stents were found to have complications, versus 0 of 17 children without stents (20% vs. 0%, p=0.05). Two patients required readmission for febrile UTI, 2 had dysuria, and 2 had stent displacement. Complete resolution of hydroureteronephrosis was shown in 45/47 (96%) patients in 14.7±6.22 mos. No ureteric dilation was seen on post-operative ultrasound at last F/U. Persistent hydronephrosis (Grade II-III) remained in 1/30 (3%) stented and 1/17 (6%) stentless patients at last F/U. No difference was found between stented and stentless U-U in operative time, hospital stay, and time to resolution of hydronephrosis.
CONCLUSIONS:
Stented U-U was associated with increased patient morbidity, including UTI, discomfort and hospital readmission compared to stentless cases. Based on that, we believe stenting may not be necessary during U-U for repair of upper-pole ectopic ureters.
Back to 2014 Fall Congress Meeting Posters
|