Combined spinal/caudal catheter anesthesia: Extending the boundaries of regional anesthesia for complex pediatric urological surgery
Venkata R. Jayanthi, MD1, Kristen Spisak, MD2, Ashley E. Smith, MD1, David P. Martin, MD1, Christina Ching, MD1, Tarun Bhalla, MD1, Joseph D. Tobias, MD1, Emmett Whitaker, MD1.
1Nationwide Children's Hospital, Columbus, OH, USA, 2Dayton Children's Hospital, Dayton, OH, USA.
Background: Spinal anesthesia (SA) is an established anesthetic technique for short outpatient pediatric urological cases. In order to avoid general anesthesia (GA) and expand regional anesthetics to longer and more complex pediatric surgeries, we began a program using a combined spinal/caudal catheter technique (SCC).
Methods: We reviewed the charts of all patients scheduled for surgery under SCC between December 2016 and April 2018 and recorded age, diagnosis, procedure, conversion to GA/airway intervention, surgery time, neuraxial and intravenous medications administered, complications and outcomes. The SCC technique usually involved an initial intrathecal injection of 0.5% isobaric bupivacaine followed by placement of a caudal epidural catheter. Patients received 0.5 milligrams-per-kilogrammg/kg of oral midazolam approximately 30 minutes prior to entering the operating room, at the discretion of the anesthesiologist. One hour after the intrathecal injection, 3% chloroprocaine was administered via the caudal catheter to prolong the duration of surgical block. Intraoperative management included either continuous infusion or bolus dosing of dexmedetomidine for patient comfort and to optimize surgical conditions. Prior to removal of the caudal catheter in the post-anesthesia care unit, a supplemental bolus dose of local anestheticesia was given through the catheter to provide prolonged post-operative analgesia.
Results: Overall, 20 children underwent attempted SCC. SA was unsuccessful in 3 patients and they were converted to GA. The remaining 17 children all had successful SCC placement, and their average age was 17.2 months (range 3.3 – 43.8 mos.). Of the 17 surgeries performed under SCC, there were 11 open ureteral reimplantations, 2 first stage hypospadias repairs, 1 second stage hypospadias repair, 2 feminizing genitoplasties for congenital adrenal hyperplasia, and 1 open pyeloplasty. Average length of surgery was 108 minutes (range 68 – 172 min). 13/17 (76%) did receive preoperative midazolam and16/17 (94%) had continuous infusion of dexmedetomidine intraoperatively with boluses as needed. All SCC patients were spontaneously breathing room air during the operation and there were no airway interventions. Only one SCC patient received opioids intraoperatively. There were no intra or perioperative complications.
Conclusion: SCC allows for complex surgeries to be performed exclusively under regional anesthesia, thus obviating the need for airway intervention, minimizing or eliminating the use of opioids, and avoiding known and potential risks associated with general anesthesia. The latter is of particular importance given current concerns regarding hypothetical neurocognitive effects of GA on children under 3 years of age. 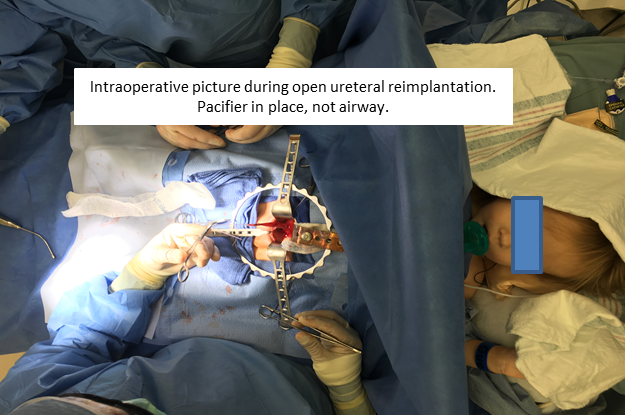
Back to 2018 Program




