Stone Formation and Bacteriology after Bladder Augmentation in Bladder Exstrophy
Jason Michaud, MD, PhD, John Jayman, BA, John Gearhart, MD.
Johns Hopkins School of Medicine, Baltimore, MD, USA.
BACKGROUND
Intestinal bladder augmentation (enterocystoplasty) can predispose patients to urinary stone formation. This risk is further complicated when coupled to the frequent use of continent urinary diversion. Furthermore, patients with the Exstrophy-Epispadias Complex (EEC) of conditions require bladder augmentation with increased frequency, owing to major bladder dysfunction and incontinence. Given the risk of stone formation in this population, we sought to examine stone formation and management, at our institution. In addition, we sought to explore the potential influence of urinary bacteria on stone formation in this group.
METHODS
We performed a retrospective review of EEC patients who underwent intestinal bladder augmentation, or continent urinary diversion with intestinal segments, at the author’s institution between 1980 and 2017. Data collected included demographics, surgical management, stone pathology, and urine cultures associated within 3 months of stone procedures.
RESULTS
A total of 324 patients underwent intestinal bladder augmentation from 1980-2017. Sigmoid colon and ileum were equally utilized for augmentation (46% each), with 8% of augmentations using both colon and ileum. Ninety-eight percent of patients underwent both continent urinary diversion and bladder augmentation. One hundred and one patients (31%) developed stones, within a median follow-up of 6.3 years. The majority of stones (79%) formed within the augmented bladder. There was no association between the type of augmentation or diversion and stone formation. Patients underwent a median of 2 stone procedures during follow-up (range 1-11). Percutaneous cystolithalopaxy was the most common form of stone extraction (41%) followed by stomal cystoscopy (27%) and open extraction (21%). Fifty patients (15%) were recurrent stone formers requiring two or more stone procedures. Stone composition was highly variable, and mixed composition stones were common. Struvite stones were more common among recurrent stone formers (p = 0.01). Recurrent stone formers were also more likely to have a history of stone formation in their kidney or bladder pre-augmentation (p= 0.01).
Urinary bacterial profiles among stone formers, as a whole, were highly variable. There were, however, distinct profiles of bacterial growth in the urine of recurrent stone formers (Figure 1). Notably, patients with recurrent stones were more likely to grow Proteus mirabilis and Enterococcus faecalis on urine culture (p= 0.04). In contrast, patients with a single stone event were more likely to grow Staphylococcus aureus (p= 0.04).
CONCLUSIONS
One-third of EEC patients undergoing intestinal bladder augmentation will go on to form stones, with the majority forming within their augmented bladder. A subset of patients will require repeated procedures for stone formation, most commonly percutaneous cystolithalopaxy. Although struvite stone formation remains a common cause of recurrent stone formation in the EEC population, non-urease producing organisms such as enterococcus are more commonly found in the urine among recurrent stone formers. In
addition, bacterial growth profiles differ among patients who form stones recurrently. Together these results suggest that alterations in urinary bacterial flora following augmentation may contribute to stone formation. 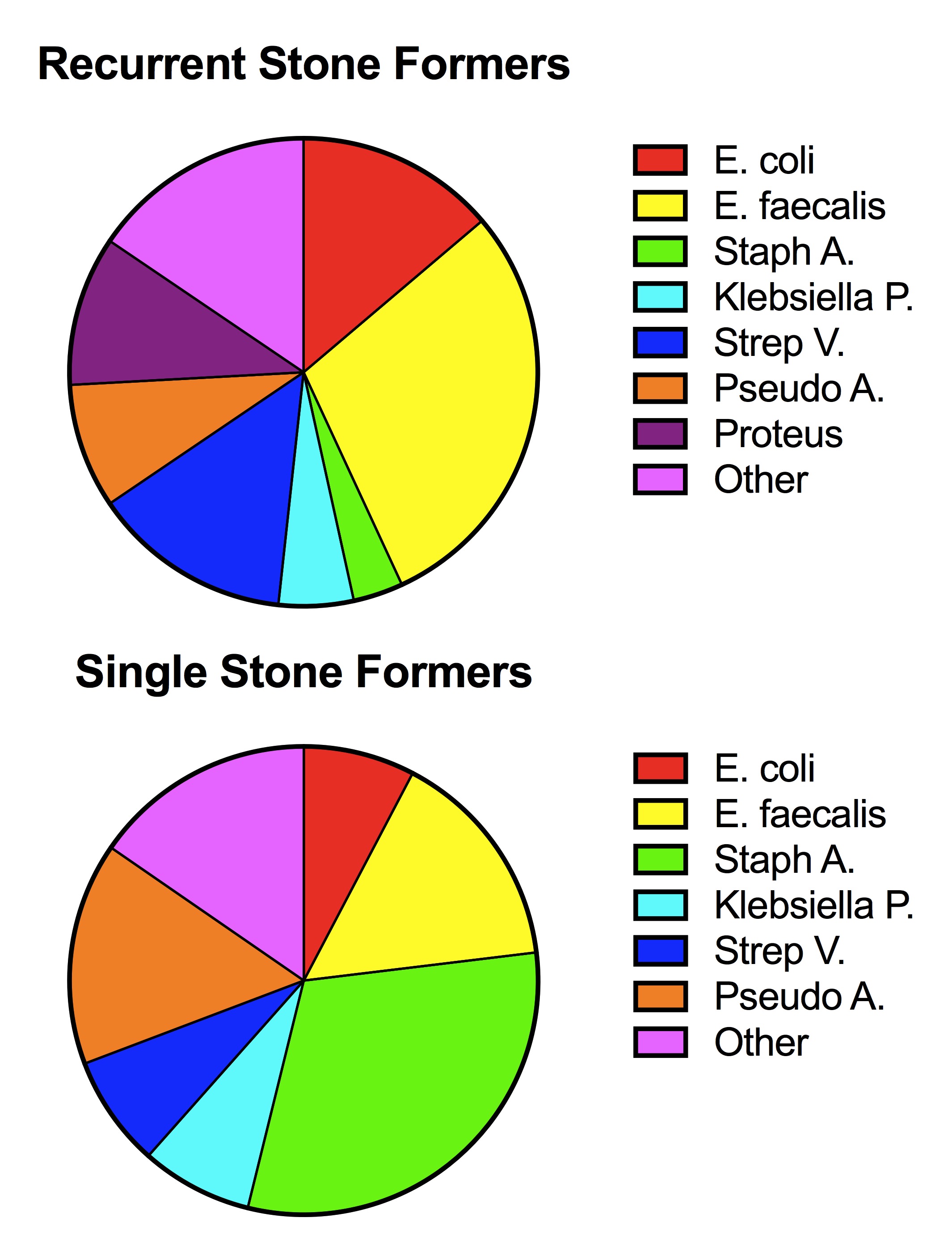
Back to 2018 Program




