Reduction in voiding cystourethrograms after pediatric urinary tract infection without increase in adverse outcomes using a clinical standard pathway
Courtney K. Rowe, MD, Claudia Crowell, MD, MPH, Sarah J. Lowry, PhD, Claudia Berrondo, MD, Paul A. Merguerian, MD, MS.
Seattle Children's Hospital, Seattle, WA, USA.
BACKGROUND: The American Academy of Pediatrics (AAP) introduced new guidelines on voiding cystourethrogram (VCUG) for patients with urinary tract infections (UTI) in 2011 raising concerns that there would be a resultant increase in missed or delayed diagnoses of significant vesicoureteral reflux (VUR). At our institution, an evidence-based pathway for pediatric UTI was developed by a multidisciplinary clinical working group and has been used since June 2010 with recommendations that align with the AAP guidelines. We set out to understand the impact of this pathway on VCUG rates after UTI and impact on VUR diagnoses and surgery. We hypothesized that VCUG rates would decrease with no significant delay in diagnosis of VUR or delay in progression to surgery.
METHODS: We reviewed prospectively tracked patients eligible for the UTI pathway. Patients discharged from the emergency room or inpatient units with a confirmed diagnosis of UTI from 9/2008-12/2016 were included, with pre-implementation patients defined as those seen before June 2010. Exclusion criteria include history of prior UTI, chronic kidney disease, genitourinary abnormalities including known VUR or medically complicating factors. Rate of immediate VCUG (< 60 days after UTI diagnosis), rate and timing of later VCUG (≥ 60 days after UTI diagnosis), rate and timing of future VUR diagnosis and rate and timing of future VUR surgery were calculated.
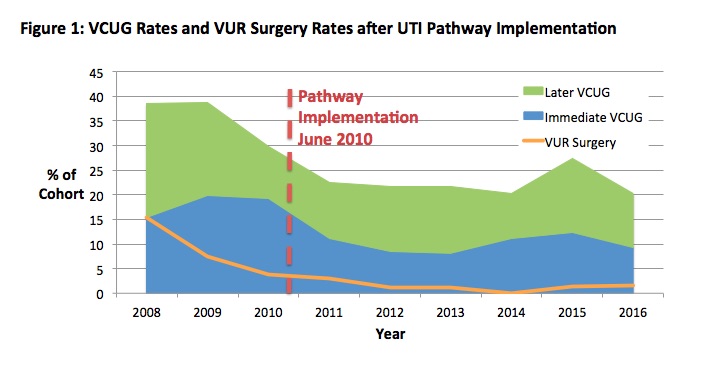
RESULTS: We identified 727 patients; 165 in the pre-implementation period and 562 in the post-implementation period (Table 1). There was a statistically significant decrease in the proportion receiving VCUGs after the first UTI (20.0% vs. 11.0%, p = 0.003). The rate of later VCUG also decreased but not significantly (16.4% vs. 12.3%, p = 0.173). Future VUR diagnosis and future VUR surgery rates decreased after implementation, as did time from first UTI to diagnosis of VUR. For those who went on to VUR surgery, there was no significant change in time from first UTI to surgery (mean 12.8 months vs. 19.0 months, p = 0.418).
CONCLUSIONS: While VCUG rates decreased after implementation of the UTI pathway, there is no evidence that patients had a delay in diagnosis or treatment of VUR or that there was an increase in missed diagnoses of surgically significant VUR. Limitations include ED and inpatient inclusion criteria and the national trend towards fewer VCUGs and fewer surgical interventions in this population. Our study illustrates that standardized pathways based on evidence and national guidelines can reduce imaging interventions without sacrificing high quality of care for patients. 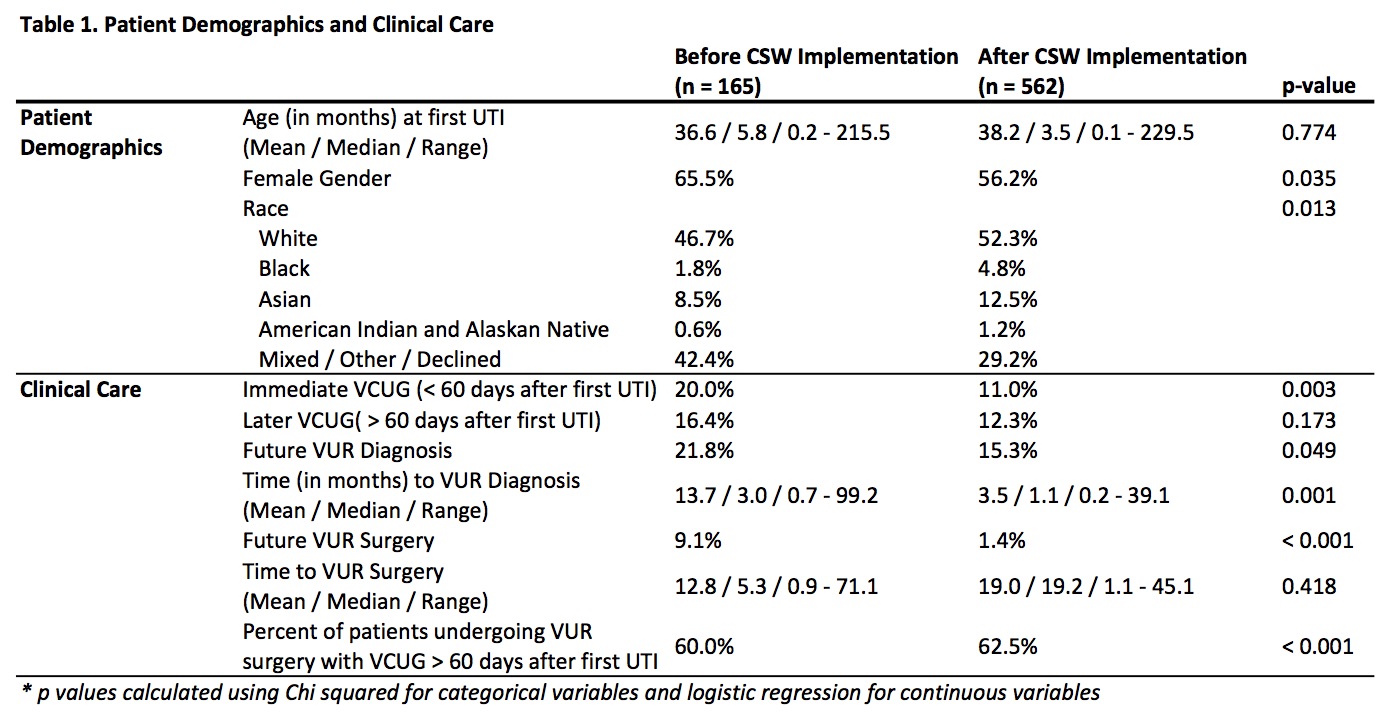
Back to 2018 Program




