Post-obstructive bladder smooth muscle remodeling is dependent on bladder mesenchymal stem cells
Belinda Li, MD, Megan Y. Devine, BS, Nicholas M. Tassone, BS, Paulette M. Hausner, BS, Robert W. Dettman, PhD, Edward M. Gong, MD.
Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, USA.
BACKGROUND: Despite surgical correction, posterior urethral valves can lead to long-term progressive bladder dysfunction. This natural history may indicate an abnormal bladder stem cell population as a result of partial bladder outlet obstruction. Using a murine model, a Sca-1+/CD34+ coexpressing mesenchymal stem cell population was previously identified in the stromal layer of the bladder which is altered after acute and partial outlet obstructions. Smooth muscle gene expression was similarly found to be downregulated after obstruction. Our objective is to study the function of bladder stem cells in response to injury by outlet obstruction. We hypothesize that loss of Sca-1 will affect the physiologic detrusor hypertrophy that occurs after obstruction, leading to changes in compensatory function.
METHODS: 6-8 week-old male Sca-1 null (Sca1KO) mice and genetically unmodified C57BL/6 (WT) mice both underwent surgical partial obstruction (PO) at the bladder neck. An additional cohort of Sca1KO mice underwent sham surgery for comparison. Voiding stains on paper (VSOP) at 1, 2, and 4 weeks were quantified for functional assessments of the bladder. Whole bladders were excised at 4 weeks and distributed for histologic exam. Bladder thickness, weight, and circumference were measured. Masson's Trichome staining was used to calculate detrusor collagen to smooth muscle ratios and total smooth muscle content. Identification of DNA synthesis in proliferating cell types in response to intervention was performed by immunofluorescence imaging of 5-ethynyl- 2’-deoxyuride (EdU) incorporation at various time points of post-operative days (POD) 1, 4, and 8.
RESULTS: After PO compared to sham, Sca1KO mouse bladders on average had significantly increased bladder circumference (1.9 vs 1.1cm), bladder weight (48.7mg vs. 31.2mg), and collagen-to-smooth muscle (C:SM) ratio (0.56 vs. 0.17). Comparing WT to Sca1KO mice after PO, Sca1KO PO bladders had increased fibrosis, or collagen-to- smooth-muscle ratio (0.48 vs. 0.38, p=0.0386), and decreased smooth muscle content by weight (41.61 vs 65.62mg, p=0.0554). EdU labeling showed increasing cellular proliferation in WT PO bladders over time whereas proliferation in Sca1KO PO bladders declined by POD8. Of EdU-staining cells at POD8, those co-staining with calponin comprised 0.60 in WT mice compared to 0.02 in Sca1KO mice, though the result was not statistically significant (p=0.12).
CONCLUSIONS: Loss of Sca-1 does not appear to affect normal bladder function. In response to injury with PO, Sca1KO mouse bladders displayed decreased smooth muscle hypertrophy and increased collagen infiltration consistent with fibrosis compared to stem cell-intact comparisons. 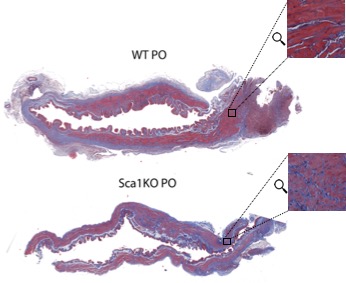
Back to 2018 Program




